Hearing Aid Fitting Tips | November 2003 Hearing Review
By Francis Kuk, PhD, Denise Keenan, MA, and Carl Ludvigsen, MS
Editor’s Note: Unfortunately, some of the images in the online version of this article were deleted when we converted to a new web format. You can download a PDF of this article if you wish to see the graphics and read the original article as it appeared in the magazine.
A low frequency sensorineural hearing loss—sometimes called a “reverse-slope audiogram”—is one of the more difficult-to-fit audiometric configurations. Although many researchers1,2 have proposed solutions to manage this hearing loss configuration, some of these solutions were not fully achievable because of the limitations of the hearing aid technology at the time. With the advent of digital multichannel nonlinear hearing aids that offer greater flexibility of adjustment and increased specificity, a clinician may experience enhanced success in managing this loss configuration. This article reviews some of the challenges involved in fitting reverse-slope hearing loss.
Why Does Low-Frequency Hearing Loss Pose Unique Challenges?
Hard to Identify. Unless a person has a familial history of low frequency hearing loss or he/she undergoes routine audiometric testing, this type of hearing loss is not easily identified because it is relatively symptom-free. One reason is that low frequency sounds are more intense and carry less information than high-frequency sounds. A person with a moderate degree of low frequency hearing loss may not exhibit any outward signs of a hearing loss, such as missing speech sounds or aberrant speech production patterns.
Relatively intact intelligibility in quiet. One reason why people with a low frequency hearing loss are able to identify the low-frequency speech information is because low frequency information may also be carried by high frequency fibers through temporal coding. Thornton & Abbas3 compared the speech recognition ability of 3 subjects who were identified with a low frequency dead region and 5 normal-hearing individuals in various filtered conditions. In the unfiltered condition, the speech scores were 56% to 88% for the impaired group and 94% to 100% for the normal-hearing group. For the high-pass condition, the scores were 34% to 46% for the hearing-impaired group but 16% to 38% for the normal-hearing group. For the low-pass condition, the scores were 12% to 44% for the hearing-impaired group but 76% to 84% for the normal-hearing group.
These findings suggest that amplifying the low-frequency dead region alone may not result in improved speech understanding. In addition, it suggests that people with a low frequency hearing loss may be able to utilize the surviving mid- and high-frequency hearing as effectively, if not more effectively, than normal-hearing subjects. Van Tasell & Turner4 reached similar conclusions. From a practical standpoint, this means that the application of a prescriptive target where the amount of gain is directly proportional to the degree of hearing loss may lead to less than satisfactory results in many wearers.
High expectations for hearing aids. Because of their ability to utilize mid- and high-frequency signals, many adults who are born with a low frequency hearing loss develop normal speech and language skills. Although they may have some difficulties in groups or in noisy environments, many of these individuals have learned to manage their communication. As a result, even when these individuals agree to try hearing aids, they may have unrealistic expectations for the chosen devices and reject any attempts that may be less than perfect.
Diverse etiologies and expression of symptoms. Unlike a high frequency hearing loss where a majority of cases are related to prolonged exposure to loud sounds and aging, a low frequency hearing loss is typically not related to the same factors. Rather, hereditary and/or genetic origin is a common cause of a low frequency hearing loss. For example, Konigsmark et al.5 reported that a progressive low frequency hearing loss may be dominantly inherited. Lesperance & Burmeister6 reported that Wolfram Syndrome 1 (an autosomal recessive disorder) is a result of mutation in the WSF1 gene. Some patients who have Mondini dysplasia may be born with no functional Organ of Corti in the apex of the cochlea.7
A low frequency hearing loss may also be related to disease processes that affect the integrity of the hair cells in the apex of the cochlea. Sudden hearing loss,8 viral infection,9 renal failure,10 and Meniere’s disease11 have been associated with a low frequency hearing loss. Changes in the endolymphatic pressure, as in cases with fistula,12 intracranial hypertension,13 and even spinal and general anesthesia14 have also been reported with varying degrees of transient and permanent low frequency hearing loss. The diverse etiologies, permanence (transient vs permanent vs progressive), and severity (moderate to profound) would suggest that one should understand the etiology of a particular patient’s hearing loss in order to customize management.
Difficulties in Amplifying the Low Frequencies
Potential dead region. Gravendeel & Plomp15 first suggested that a moderate degree of low frequency hearing loss may be associated with a dead region—a frequency region where no surviving inner hair cells may be found. This suspicion was confirmed subsequently by researchers through the use of psychophysical tuning curves and/or masking studies.3,4,15 Humes et al.17 suggested that a reverse slope audiogram with a slope at the rising portion of the audiogram that exceeds -25 dB/octave may suggest a dead region. Moore18 indicated that a hearing loss which exceeds 50 dB HL in the low-frequency region, with normal-to-mild hearing loss in the mid-to-high frequencies, may indicate a dead region.
If, indeed, the low frequency region is dead, amplifying this frequency region—like amplifying a high frequency dead region—may not improve the wearer’s speech intelligibility. Instead, amplifying the nearby mid- and high-frequency fibers may improve intelligibility. This was evidenced in the reports of researchers such as Thornton & Abbas3 and van Tasell & Turner.4 Subjectively, a dead region may not yield any tonal perception19 and exhibit poor frequency discrimination. However, Moore18 reported erratic results on pitch perception in low frequency dead regions.
Improved sound quality—with trade-offs. Even assuming that the low-frequency region is not “dead,” there are consequences to amplifying the low frequencies. On the positive side, amplifying the low frequencies will improve audibility of weak low frequency sounds and result in an increase in loudness and an improvement of sound quality.20,21 Yet, having too much low frequency output may mask the audibility of the mid and high frequency sounds.22 Furthermore, over-amplification in the lows can result in a higher ambient noise level and an increased susceptibility for noise interference. Unfortunately, with linear hearing aids, it may be difficult to provide just the right amount of low frequency amplification to ensure audibility without over-amplifying higher inputs. This over-amplification can lead to higher frequencies being compromised by the upward spread of masking, and a decrease in intelligibility and sound quality.
Need for occluded earmold/shell. In order to retain the low frequency output of a hearing aid, the earmold/shell must be occluding with minimal leakage or vents. An increase in leakage (or vent diameter) will decrease the amount of low-frequency output measured in the ear canal. For example, a 2 mm vent diameter will reduce the low-frequency output by as much as 13 dB at 250 Hz.23 Thus, to preserve the low-frequency output, a completely occluding earmold/hearing aid should be used. In addition to preserving the output, an occluded earmold also preserves the directivity index of a directional microphone.24
However, use of an occluded earmold increases the likelihood of the occlusion effect. It is possible that the wearer will find his/her voice “echoic” or “hollow” with a closed earmold. Increasing the vent diameter (or leakage) could reduce the physical occlusion effect when the wearer speaks.25 A compromise on venting is necessary between achieving the desired low frequency output and minimizing any potential occlusion effect. Alternatively, methods to manage occlusion should be available to achieve the low frequency amplification without compromising the benefits of the other features of the hearing aids and affecting the wearer’s voice quality.
In summary, it is difficult to identify and to convince patients who have a low frequency hearing loss that they need to wear hearing aids. This is mitigated by the fact that some of these patients may have a dead region in the low frequencies where amplification may not result in any improvement. On the other hand, even if that region is not “dead,” over-amplifying the low frequency region may have the undesirable consequence of loudness intolerance and masking.
| Two Case Studies: Examples of Using Paired Comparisons for Customization of Fittings
By using the paired comparison technique, we can systematically change the bandwidth and gain in discrete steps in order to estimate the optimal bandwidth and preferred gain at different input levels. This allows one to examine if these patients would prefer a broader bandwidth (versus low-pass and high-pass) than their audiogram would indicate, and if their gain preference at different input levels is similar to patients with more typical audiometric configurations. This technique may account for individual differences in etiology of loss as well as preferences for specific sound quality.
A Case with Tonal Perception During the paired comparison task, the hearing aids were first set to the default settings. The Connected Sentence Test (CST) was presented at 45 dB HL (approximately 65 dB SPL), and Subject A was asked to adjust the insertion gain setting for conversational sounds (IG normal) at each of the four basic frequency channels, starting at 500 Hz and proceeding to 1000, 2000, 4000, and then 500 Hz. She compared the default settings with alternate settings (more or less gain) until she had the best speech understanding with the best sound quality. She was then asked to listen to a different passage at a presentation level of 25 dB HL and adjust the gain parameter for soft sounds (IG soft) in the four frequency channels. Her instructions were to select the best gain settings so that the sounds are audible and soft, but not necessarily intelligible. Finally, she was asked to listen to a discourse passage presented at 65 dB HL and instructed to adjust the gain parameter for loud sounds (IG loud) so that the passage was loud, but not uncomfortable.
Figure 4 compares the simulated in-situ frequency-output curves at the input levels of 40 dB, 65 dB, and 90 dB SPL between the prescribed default settings (left) and the self-selected settings (right). Several observations are evident. First, the frequency-output for the 40 dB SPL input level was similar between the two settings. That is, Subject A selected similar gain as recommended by the proprietary fitting algorithm. The default setting attempts to bring the aided sound-field threshold at all frequencies to about 20 dB HL in the ideal situation. Secondly, significantly higher output than the default setting was selected for the 65 dB SPL input level condition in the 250-500 Hz region, while a lower output was selected in the 1000 Hz region. This is opposite to our expectation and that of other researchers (eg, Moore18). In previous studies, subjects with almost identical hearing loss typically preferred less gain in the low frequencies and more gain in the mid frequencies at the 65 dB SPL input level condition. For the 90 dB SPL input level, the self-selected setting is slightly lower than the default setting predicted from Pascoe’s findings28 on the relationship between UCL and the degree of hearing loss. Subject A reported no occlusion problem with either the default settings or the self-selected settings. Speech recognition scores for the default settings were similar to the self-selected settings in both quiet and noisy situations. Although Subject A liked both settings, she preferred the self-selected settings. A Case with “Atonal” Perception
Subject B completed the same fitting protocol as Subject A. Figure 5 compares the frequency-output curves at the 3 input levels between the default settings and the self-selected settings. Again, several observations are clear. First, the self-selected frequency output curve at the 40 dB SPL input level was similar between the default and self-selected settings. This suggests that, even though 250 Hz may sound atonal, the subject still preferred the default gain for soft sounds in the nearby frequency region. On the other hand, the preferred gain for the low-frequency at 65 dB SPL and 90 dB SPL input levels was lower than that recommended by the default setting, whereas the output in the 2000 Hz-4000 Hz region was higher for the self-selected settings than the default settings. Her speech-in-noise score (as evaluated by the HINT) was significantly better with the self-selected settings than with the default settings. Subject B did not report any occlusion problem. Although she preferred the Senso Diva over her Senso C9+, she still reported that the low-frequency sounds appeared “plain” and “atonal.” |
What Has Been the Strategy for Management of LF Losses?
Previous research on the management of a low frequency hearing loss focused on two main issues: 1) the identification of a dead region, and 2) the assignment of optimum frequency-gain characteristics on the hearing aids.
Assessing the status of the hearing loss region. In the previous section we reviewed the audiometric characteristics of a low frequency hearing loss with a dead region.17,18 There are also tools that directly measure the functional status of the low frequency fibers.
Halpin et al.2 examined the effect of ipsilateral pure-tone masking of the basal fibers (higher frequencies) at a high stimulus level (80-90 dB HL) while re-determining the audiogram of the low frequencies. An increase in thresholds in the low frequencies will occur if the responses are mediated by the higher frequency fibers. Moore & Alcantara16 recommended the use of psychophysical tuning curve to determine the status of the low frequencies. In an effort to make the test more clinically feasible, Moore18 proposed the use of the Threshold Equalizing Noise (TEN) as a quick means to assess the functional status of the low frequency region.
One can also compare word-recognition scores with the predicted Articulation Index (AI) scores with and without the low frequency contribution in order to estimate functional status.2 If the low frequency fibers are functional, the measured word recognition scores should change according to the predicted AI scores when the low frequency contribution is included. Otherwise, the measured word scores would not be affected by the low frequency contribution.
Amplifying the region of loss. Deciding on the frequency region to amplify and how much to amplify are not as easy. Schum & Collins1 examined speech-recognition skills of 6 subjects with a low frequency hearing loss by spectrally shaping speech materials (NST and CCT) to approximate different amplification schemes. These included: a) unaided; b) low-pass filtering; c) high-pass filtering; and d) broadband amplification. Their results showed that “low-pass” had the lowest intelligibility rating (4/10) and “broadband” had the highest rating (7.5/10). This suggests that amplifying the low frequency alone (or region of hearing loss alone) is not sufficient. A broadband approach, where a nearby frequency region is amplified, is desirable. These findings are in line with the observations of Thornton & Abbas3 and van Tasell & Turner.4 Moore18 suggested that “possibly amplification should be applied over a frequency range extending somewhat into the dead region…” However, the extent into the dead region and how much to amplify will probably depend on the etiology of the low frequency hearing loss. Despite these recommendations, a practical approach to customize the individual fittings with linear hearing aids has been difficult.
In summary, the current thinking on managing a low-frequency hearing loss would support broadband amplification instead of low-pass filtering. In this way, both the low frequency fibers and the mid-to-high frequency fibers can be stimulated. Furthermore, many would support the use of a large vent or open mold to reduce the low frequency output and minimize the incidence of loudness intolerance, upward spread of masking, and potential occlusion.
Digital Technology and New Options for LF Losses
One difficulty in the management of low frequency hearing loss is predicting the appropriate level-dependent frequency-gain characteristics based on the audiogram. The second is the difficulty in achieving the recommended characteristics. New DSP hearing aids allow:
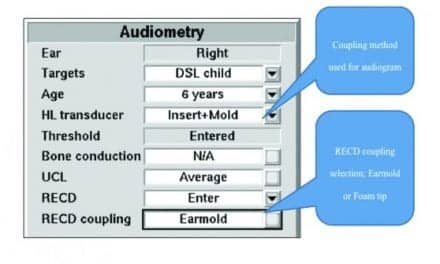
.gif)
1. Increased sophistication in nonlinear signal processing to ensure audibility and comfort. Until the last 10 years, the majority of hearing loss was managed with linear amplification. A defining characteristic of linear processing is that the same gain is applied to all input levels. This means that the effect of gain adjustment will be felt for sounds at all input levels. If someone with a low-frequency hearing loss desires less than the prescribed gain (eg, because of loudness intolerance), such gain reduction will occur for all input levels. Figure 1 is an input-output (I-O) curve of a linear hearing aid where the gain curve has been lowered from 40 dB to 20 dB in order to avoid discomfort at high input levels, a common complaint of people with a reverse-slope audiogram. It is obvious that not only the output at a high input level is reduced, but the output at other input levels is reduced as well. This sacrifices the audibility of soft sounds and potentially compromises sound quality at conversational levels. If one recognizes that the problems associated with masking, occlusion, loudness intolerance, and difficulty in noise are all related to a high output (from amplifying high input levels) in the wearer’s ears, one should only reduce gain for high input level sounds and not gain for sounds at all input levels.
The use of nonlinear or compression hearing aids can ensure audibility while maximizing comfort for the wearer. As a rule, a nonlinear hearing aid provides decreasing gain as input level increases. Furthermore, some nonlinear hearing aids allow clinicians to adjust gain for different input levels (soft, medium and loud) independently. An advantage of using digital nonlinear hearing aids is that gain adjustment at more discrete input levels can be made. This means that one may control gain just for loud sounds without sacrificing gain for soft and medium level sounds.
.gif)
One advantage of using digital nonlinear hearing aids over linear ones is seen in the hypothetical input-output (I-O) curve of the Senso Diva hearing aid in Figure 2. This hearing aid allows gain to be adjusted at three ranges of input levels: “IG soft” for sounds below 50 dB, “IG normal” for sounds between 40 and 60 dB, and “IG loud” for sounds above 50 dB. For an individual with a 50 dB hearing loss in the low frequency, one can ensure comfort while maintaining audibility for soft sounds by reducing gain for loud inputs only. In this example, only output above a 50 dB input level is affected. Sounds as soft as 10 dB are audible (whereas before, sounds are audible only above 30 dB) and sounds below 100 dB are within the comfortable range. Thus, audibility is not sacrificed to achieve comfort. Moore18 also recommended the use of nonlinear WDRC hearing aids for people with a low frequency hearing loss.
2. Increased specificity of frequency processing (increased number of channels). In general, as the number of channels in a hearing aid increases, the specificity at which one can limit the type of processing to a restricted frequency region increases. This is often helpful in a reverse-slope audiogram where the change in threshold between octaves is rather abrupt. Indeed, a steep audiogram slope is one indication of a “dead” region.18 In a single-channel device, minimizing gain for the low frequencies may be compromised by the need to provide gain to nearby frequencies. Having multiple channels in a nonlinear hearing aid allows one to provide appropriate amplification at one frequency region without over-amplifying (or under-amplifying) nearby frequency regions.
3. Noise reduction strategies to manage speech understanding in noise. One of the main concerns of people with a low frequency hearing loss is their difficulty understanding speech in noise. The problem may be exacerbated when the wearer is given significant amount of gain in the low frequencies. In this case, it would be desirable to have hearing aids that deliver the required amount of low frequency gain for soft sounds in quiet but are also capable of automatically reducing their gain/output in noise. Many DSP hearing aids have noise reduction algorithms and adaptive directional microphones that minimize the impact of noise.22
4. Capability for individual tailoring. Due to etiologies, one challenge in managing a low frequency hearing loss is the difficulty in predicting the desired frequency-gain. Moore18 acknowledged that, even when one makes a diagnosis of a dead region, the amount of amplification one provides to the dead region and to the mid- and high-frequency region is still unclear. The recommended frequency-gain characteristics should be customized to the individual. A tool that allows this customization is desirable.
One advantage of digital technology is the capability to save alternate settings of the hearing aids into a temporary memory for comparison of preference. These settings can be compared in pairs adaptively in the clinic in order to zero-in on the optimal settings for the wearer. For example, the bandwidth and gain of the hearing aids at each input level may be adaptively changed based on the wearer’s preference. Alternatively, the clinicians can save different combinations of settings into the different memories of the hearing aids and have the wearer evaluate their relative performance in real-life situations. This ability to allow paired comparisons27 in digital and programmable aids will be especially helpful to select the optimal level-dependent frequency-gain settings on a hearing aid for people with a low-frequency hearing loss (and other hearing loss configurations as well). This is demonstrated in two case studies on page 36.
Summary
With the increased flexibility and specificity of digital processing, and with the use of new fitting tools (eg, paired comparison), one may conclude that:
- A digital multichannel nonlinear hearing aid has more features than a linear hearing aid to match the gain requirement of people who have a low-frequency hearing loss;
- Use of wide dynamic range compression (WDRC) with a low compression threshold (CT) and high level compression may be more effective (than linear or WDRC with high CT) in preserving audibility and maintaining comfort across listening environments;
- People with a reverse-slope audiogram do prefer amplification in the low frequency. However, their gain preference, compared to the recommendations of some proprietary fitting targets, may vary depending on input levels.
- A broad bandwidth, including amplification in the normal or near-normal frequency region, is desirable. However, the specific amount needs individual customization;
- The paired comparison technique may help customize individual settings.
Francis Kuk, PhD, is director of audiology, and Denise Keenan, MA, is an assistant research audiologist at the Widex Office of Research in Clinical Amplification-USA, Lisle, Ill; Carl Ludvigsen, MS, is manager of audiological research at Widex A/S, Vaerloese, Denmark. |
Correspondence can be addressed to HR or Francis Kuk, PhD, Widex Hearing Aid Co, 35-53 24th St, Long Island City, NY 11106-4116; email: [email protected].
References
1. Schum D, Collins J. Frequency response options for people with low-frequency sensorineural hearing loss. Am J Audiol. 1992;11:56-62.
2. Halpin C, Thornton A, Hasso M. Low-frequency sensorineural loss: Clinical evaluation and implications for hearing aid fitting. Ear Hear. 1994;15:71-81.
3. Thornton A, Abbas P. Low-frequency hearing loss: Perception of filtered speech, psychophysical tuning curves, and masking. J Acoust Soc Am. 1980;67, 638-643.
4. Van Tasell D, Turner C. Speech recognition in a special case of low-frequency hearing loss. J Acoust Soc Am. 1984;75:1207-1212.
5. Konigsmark B, Mengel M, Berlin C. Familial low frequency hearing loss. Laryngoscope. 1971:81(5):759-71.
6. Lesperance M, Burmeister M. Gene Identified for low-frequency hearing loss. Hear Jour. 2002;55(3):8.
7. Parving A. Inherited low-frequency hearing loss. A new mixed conductive/ sensorineural entity? Scand Audiol. 1984;13(1):47-56.
8. Mattox D, Simmons E. Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol. 1977;86:463-480.
9. Djupesland G, Flottorp G, Degre M, Stein R, Skrede S. Cochlear hearing loss and viral infection. Acta Otolaryngol (Stockh). 1979;87:247-254.
10. Gatland D, Tucker B, Chalstrey S, Keene M, Baker L. Hearing loss in chronic renal failure: hearing threshold changes following hemodialysis. J R Soc Med. 1991;84:587-589.
11. Paparella M. The cause (multifactorial inheritance) and pathogenesis (endolymphatic malabsorption) of Meniere’s disease and its symptoms (mechanical and chemical). Acta Otolaryngol. 1985;99(3-4):445-451.
12. Goodhill V. Sudden deafness and round window rupture. Laryngoscope. 1971;81:1462-1469.
13. Sismanis A. Otologic manifestations of benign intercranial hypertension syndrome: Diagnosis and management. Laryngoscope. 1987;97:1-17.
14. Schaffartzik W, Hirsch J, Frickmann F, Kuhly P, Ernst A. Hearing loss after spinal and general anesthesia: A comparative study. Anesth Analg. 2000;91(6):1466-72.
15. Gravendeel D, Plomp R. Perceptive bass deafness. Otolaryng. 1960. 51:549-560.
16. Moore B, Alcantara J. The use of psychophysical tuning curves to explore dead regions in the cochlea. Ear Hear. 2001; 22(4):268-78.
17. Humes L, Tharpe A-M, Bratt G. Validity of hearing thresholds obtained from the rising portion of the audiogram in sensorineural hearing loss. J Speech Hear Res. 1984; 27(2):206-11.
18. Moore B. Dead regions in the cochlea: Diagnosis, perceptual consequences, and implications for the fitting of hearing aids. Trends Amplif. 2001; 5: 1-34.
19. Florentine M. Tuning curves and pitch matches in a listener with a unilateral, low-frequency hearing loss. J Acoust Soc Amer. 1983; 73:961-965.
20. Punch J, Beck E. Low-frequency response of hearing aids and judgments of aided speech quality, J Speech Hear Dis. 1980; 45:325-335.
21. Punch J, Beck L. Relative effects of low-frequency amplification on syllable recognition and speech quality. Ear Hear. 1986; 7:57-62.
22. Studebaker G, Sherbecoe R, McDaniel D, Gwaltney C. Monosyllabic word recognition at higher-than-normal speech and noise levels. J Acoust Soc Am. 1999; 105(4): 2431-2444.
23. Lybarger S. Earmolds. In: Katz J, ed. Handbook of Clinical Audiology. 3rd edition. Baltimore: Williams and Wilkins; 1985: 885-910.
24. Ricketts T. Directional hearing aids. Trends Amplif. 2001; 5(4):139-176.
25. Revit L. Two techniques for dealing with the occlusion effect. Hear Instrum. 1992; 43(12): 16-18.
26. Kuk F, Ludvigsen C, Paludan-Muller C. Improving hearing aid performance in noise: challenges and strategies. Hear Jour. 2002; 55(4): 34-46.
27. Kuk F. Paired-comparisons as a fine-tuning tool in hearing aid fitting. Second edition. In: Valente M, ed. Strategies For Selecting and Verifying Hearing Aid Fittings. New York: Thieme Medical Publishing; 2000: 125-150.
28. Pascoe D. Clinical measurements of the auditory dynamic range and their relation to formulas for hearing aid gain in presbyacousis and other age related aspects. In: Jensen JH, ed. Proceedings of the 13th Danavox Symposium. Danavox, Denmark; 1988; 129-147.

.gif)
.gif)
.gif) Figure 3. Audiograms of Subjects A and B.
Figure 3. Audiograms of Subjects A and B..gif) Figure 4. Comparison of simulated in-situ frequency-output curves between the default proprietary fitting and self-selected settings obtained at three input levels of 40 dB SPL, 65 dB SPL, and 90 dB SPL for Subject A.
Figure 4. Comparison of simulated in-situ frequency-output curves between the default proprietary fitting and self-selected settings obtained at three input levels of 40 dB SPL, 65 dB SPL, and 90 dB SPL for Subject A. .gif) Figure 5. Comparison of simulated in-situ frequency-output curves between the default proprietary fitting and self-selected settings obtained at three input levels of 40 dB SPL, 65 dB SPL, and 90 dB SPL for Subject B.
Figure 5. Comparison of simulated in-situ frequency-output curves between the default proprietary fitting and self-selected settings obtained at three input levels of 40 dB SPL, 65 dB SPL, and 90 dB SPL for Subject B.