Editor’s Note: There are many innovative approaches used in the field to provide exceptional service to individuals who have hearing impairment. This article is the first in a series that examines some of the unique ways dispensing professionals tackle various problems encountered in their daily work.
The model for hearing rehabilitation came from the military hearing rehabilitation centers during World War II. The name “audiology” was coined at that time. Soldier-patients were given hearing tests, and hearing aids were selected, evaluated, and provided when needed. Auditory training and auditory-visual speech perception training were given, and for some patients, speech improvement, hearing conservation, and counseling were included in the program.
About this same time, members of the American Speech and Hearing Association (now ASHA) Ethical Committee decided that the selling of hearing aids by an audiologist was unethical and that a transgressor would be expelled from the organization. An audiologist could select, evaluate, and prescribe a hearing aid, but it would have to be purchased from a hearing aid dispenser.
When, in the mid-1970s, ASHA finally decided that it was no longer a crime to sell hearing aids, audiologists began to market and dispense hearing aids, but audiology services remained a central role. Marketing is a hot topic today in our professional journals; however, very little is being said about marketing hearing rehabilitation—mostly because, when compared to hearing aids, little seems to change in hearing rehabilitation and few new ideas are being promulgated.
In the authors’ opinion, the profession that had such high aspirations and high expectations for hearing rehabilitation in those early years has now practically abandoned it in favor of hearing instrument dispensing and the impressive technology that accompanies it. If the hearing industry is serving only 22% of those who could benefit from hearing aids, it seems obvious that a return to the original concept of hearing rehabilitation is long overdue. In an effort to help revive hearing rehabilitation for audiologists, we present a hearing rehabilitation protocol with which the authors have enjoyed excellent results.
Author’s Note: The reader should recognize that this is not presented as a comprehensive assessment, selection, fitting, and verification/validation protocol—a subject that would consume far more pages than this article. Rather, the following represents the important components in what we consider to be a successful, time-tested hearing rehabilitation protocol.
Patient Interview and Basic Audiological Assessment
First, obtain a history of patients hearing problems and briefly explain the various tests that will be conducted. These include, but are not limited to:
Pure-tone Audiometry. Perform diagnostic audiometric tests for the patient as appropriate.
Speech Perception Thresholds (SRTs). For obtaining the SRTs, we recommend that Select Spondaic Words (Table 1) be used. Spondaic words with a preponderance of vowels, semivowels, and voiced consonants were selected for this list in order to avoid variability in intensity between words as occurs with words like “sunset” and “railroad.” For example, “sunset” is relatively low in intensity as compared to “railroad” which is made up completely of voiced speech sounds. Consistency in intensity increases test validity and reliability, and shortens testing time.
| 1. airplane 2. foreword 3. greyhound 4. hairbrush 5. woodwork 6. corkscrew 7. sidewall 8. doorway 9. schoolboy 10. mousetrap 11. foreground 12. doorbell 13. dovetail 14. dogwood 15. earmark 16. fireball 17. drawbridge |
18. cowboy 19. railroad 20. sailboat 21. birthday 22. hardware 23. baseball 24. grapefruit 25. proofread 26. eardrum 27. stairway 28. firebird 29. earthworm 30. forward 31. downgrade 32. playground 33. downfall 34. trademark |
35. porthole 36. fourscore 37. armchair 38. dockyard 39. wallboard 40. glowworm 41. downpour 42. foolproof 43. daybreak 44. toothbrush 45. forewarn 46. drumhead 47. doorknob 48. forehead 49. eyesore 50. wholesale |
| Table 1. Select Spondaic Words. | ||
For obtaining the SRT, use the Select Spondaic Words in the conventional manner. A total of 3 out of 5 words correct at a given intensity level is usually sufficient to establish the SRT. For obtaining the MCL and LDL, use groups of five words (or more) in a continuous sequence for each intensity level used in determining the MCL and LDL. We prefer this method for obtaining MCL and LDL over using puretones or using a continuous speech message (often strangely referred to as “cold running speech”) because we believe that it is more relevant and less time consuming than the above alternatives.
Speech Discrimination Testing. One of the reasons we humans have verbal language and speech is because we can make, consistently and at will, a great variety of sounds with our vocal cords and our organs of articulation. In English, we have 39 sounds called phonemes. The perception of these phonemes—singly or in combination with others—make words. Each phoneme plays a critical role in making speech perceptible.
It is customary for dispensing professionals to use “speech discrimination testing.” This testing is performed using half of a phonetically balanced W-22 list. In using these lists, credit is given only to words that are correctly identified; even though there may be an error for only one phoneme, no credit is given for that word. For example, for the word “fan,” the patient repeated “pan.” If “fan” was used in the context of a sentence, or while the patient was watching the speaker, such an error probably would not be made.
The lack of audibility of one or more phonemes in a word (or in several words) reduces or destroys the person’s ability to perceive the word. It is the responsibility of the hearing care professional to measure the hearing acuity of the patient for phonemes, as well as for pure-tones. Measurement of phoneme recognition cannot be accomplished through whole-word (all or none) scoring or sentence length tests. It can only be done with phoneme recognition tests.
A Phonetic Alphabet
The English language is not phonetically consistent because it contains 39 speech sounds but has only 26 letter symbols to represent them. For this reason, we find it necessary to use a phonetic alphabet which includes all of the sounds commonly used in American English. We need a phonetically consistent alphabet for recording responses in phoneme recognition testing. This alphabet proves useful for speech perception training and in discussing the rationale for speech spectrum amplification.
TABLE 2. English letters plus the above phonetic symbols make up the phonetic alphabet.
In this alphabet, letter symbols—which are often associated with particular phonemes—have been selected to represent those phonemes. For the speech sounds not assigned a regular letter symbol, new symbols have been adopted (Table 2). For example, [a] stands for the vowel sound in the word “pat” rather than for the vowel in the word “ate.” That sound has been assigned the symbol [ae]. Thus, the words “ate” and “eight” are written “aet.”
To make a simple, practical phonetic alphabet, each of the English letter symbols are assigned to only one phoneme. In some cases, two letters are assigned to one phoneme. However, in no instance have two phonemes been assigned to one letter symbol. As a result, the 39 phonemes in the phonetic alphabet are represented by 41 letter symbols (Table 3).
TABLE 3. The Phonetic Alphabet for the Phoneme Recognition Inventory and the Phoneme Recognition Quick Test. This alphabet, devised by Duffy, is made up of the regular English alphabet, the International Phonetic Alphabet, and Pitman’s Initial Teaching Alphabet. The English letter and phoneme relationship is preserved wherever possible to ease the transition from phonetic to traditional English spelling.
This phonetic alphabet provides an easy way to learn and use a symbol system for recording patient responses when taking the phoneme recognition tests. Patients who are eager to improve their speech perception can learn to identify the phonemes they seek to recognize. For each phoneme, the patient has a letter symbol that reminds them of the sound of the phoneme as well as its appearance on the speaker’s lips. This phonetic alphabet is easier to learn and less confusing than would be the case if diacritical markings were used to assign a given sound to a letter symbol.
Phoneme Recognition Testing
To truly evaluate the effectiveness of amplification for speech communication, one must discover the degree to which the sounds of speech are made audible to the patient. This can be done through phoneme recognition testing.
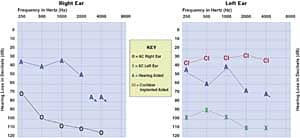
Quick Tests. With the gain control of the hearing aid to be adjusted to the most comfortable loudness (MCL) level, the patient’s phoneme recognition should be tested at the intensity level of 45 dB HL. For the patient with only a mild-to-moderate hearing loss (particularly if only in the high frequencies), the Phoneme Recognition “Quick Tests” may be all that are needed to determine phoneme recognition capability (Figure 1).
Figure 1. Sample of a Phoneme Recognition Quick Test form. This example shows the results of a patient with a slight-to-moderate hearing loss.
The Phoneme Recognition "Quick Test” presents the unvoiced consonants both when they precede and when they follow the vowel in the word. All of the vowels and unvoiced consonants of American English are represented within the 22 words of each test. A correct response for a particular consonant indicates that either the consonant was heard as it approached or receded from the vowel. When these frequencies (called transition frequencies) are audible, they often enable the patient to perceive the word or a portion of the word. By noting the patient’s correct responses, omissions, and substitutions, a record can be kept for guidance in carrying out auditory and auditory-visual speech perception training. There are two “Quick Tests” with four randomizations of each test.
Phoneme Inventories. The Phoneme Recognition Inventories are designed for patients with moderate or severe hearing impairments. Each list contains 33 words. All of the phonemes of American English appear in various vowel consonant relationships. These lists provide a generous sample for the speech-sound combinations found in everyday speech and provide a strong indication of the patient’s phoneme recognition ability.
As with the “Quick Tests,” a record of the patients responses to the Phoneme Recognition Inventories is useful in carrying out auditory and auditory-visual speech perception training. There are two “Inventory Tests,” also with four randomizations. A sample of an Inventory Test and manner of scoring is shown in Figure 2.
Figure 2. Sample of a Phoneme Recognition Inventory. This example shows the results of a patient with a moderate-to-severe hearing loss.
Acoustic Phonetics and Amplification
The voiced sounds of speech contain a fundamental tone and three formants (overtones or harmonics). Although the fundamental and first formant are important, the second formant in the vowel or semivowel is the most critical for phoneme recognition. In the vowels designated as front vowels (ie, those vowels made with the tongue toward the front of the mouth, Figure 3), the second formants appear above 1500 Hz on the frequency spectrum chart. In the vowels designated as back vowels (ie, vowels made toward the back of the mouth), the second formants appear below 1500 Hz.

Figure 3. Frequency spectrum of vowels and semivowels for average speech. Adapted from Barney.1
The significance of this information relative to the speech spectrum is that, if a patient with a moderate or severe loss has audibility restored via amplification for the frequencies below 1500 Hz, he/she can learn to recognize the middle and back vowels. If the hearing-impaired patient has audibility restored via amplification up to 3000 Hz, he/she can learn to recognize the front vowels with their high-frequency second formants, as well as all of the other vowels and semivowels.
Another significant fact is that the intensity of the speech signal is greatest for the lower frequency sounds and gradually diminishes for the higher formants. Also, with the exception of [sh] and [ch], the unvoiced consonants [p], [t], [k], [th], [f], [s], and [h] are relatively weak and have most of their identifying features between 1000 Hz-4000 Hz. The voiced consonants [b], [d], [g], [th], [v], [z], [wh], and nasals [m], [n], [ng] contain more sound energy than do the unvoiced consonants because of their low-frequency voiced components. Generally speaking, in a real-world conversation, there is a gradual decrease in the sound energy of the speech signal between 250 Hz-4000 Hz that amounts to about 20 dB.
The Speech Spectrum Curve
In keeping with the frequency/intensity relationship in the speech signal, as described above, note that the guidelines on the audiograms for the speech spectrum show a gradual rise of a total of 20 dB between 250 Hz and 4000 Hz. For maximum phoneme recognition, with the hearing aid set at the gain level most comfortable for the patient, the target area for amplification should follow the speech spectrum curve as closely as is feasible for a particular hearing loss configuration.
Soundfield Audiometry and Selective Amplification
The foundation for hearing rehabilitation is optimum audibility for the sounds needed for speech perception (while maintaining comfort for loud signals). For the hearing-impaired person, the audibility of speech sounds can only be provided through appropriate selective amplification.
Both unaided and aided threshold measurements of hearing acuity for tone and speech signals should be made in a soundfield. The aided most comfortable loudness level and the threshold of discomfort should be obtained in a soundfield with either warble tones, pulse tones, or a continuous speech signal.
The goal for the frequency/intensity characteristics and the overall gain of the hearing aid should be to make audible to the user the speech sounds most important for speech understanding. This must be done with aided soundfield measurements. In the soundfield instrumentation, we have described the true real ear measurements which can be made for the amplification characteristics of the hearing aids being considered for the patient. The dispensing professional should determine which characteristics are optimal with the speech spectrum curve rule as a guide (Figure 4a). The computer generated curve fell 10-15 dB short at 1500 Hz and 2000 Hz, a fact that could only be discovered with a soundfield measurement. Figure 4b shows the hearing aid response characteristics for a binaural fitting.


Figure 4a-B. In Figure 4a (left), it can be seen that the computer-generated curve fell 10-15 dB short at 1500 Hz and 2000 Hz, a fact that could only be discovered using soundfield measurement. Figure 4b (right) shows the hearing aid response characteristics for a binaural fitting.
A clinical audiometer and amplifier in a control room and a loud speaker in a test room are all that is required for warble tone, pulse tone, and phoneme recognition soundfield audiometry. Although auditory and auditory-visual phoneme recognition testing can be performed with live voice, recorded audiometry using an audio tape recorder/player and a VCR/TV is a more reliable procedure (Figure 5).

Figure 5. Soundfield audiometric instrumentation required for this type of testing. Capabilities include: 1) Warble tones and/or noise from audiometer, to amplifier, to speaker; 2) Live voice to audiometer, to amplifier, to speaker; 3) Audiotaped speech signal to audiometer, to amplifier, to speaker; 4) VCR audiotaped speech signal to audiometer, to amplifier, to speaker; 5) VCR videotaped speech signal to TV; 6) Client’s responses to phoneme recognition test speech signal to audiometer, to phones, to tester; and 7) Client’s responses to phoneme recognition test speech signal to audiometer, to tape recorder.
The above mentioned equipment is not highly specialized or costly, it is easy to operate, it functions efficiently, and it is very helpful in obtaining the essential information needed for effective hearing rehabilitation. In the soundfield instrumentation, a tape recorder is provided to the patient so that responses during the test may be recorded. Recorded test responses make it possible to score the test later, and provide records of progress of phoneme recognition over time. Also, these auditory and auditory-visual phoneme recognition tests can be administered by staff members other than the dispensing professional.
Soundfield tone and speech audiometry have been indispensable in the diagnosis and therapy for children and hard-to-test subjects for over 60 years. A phonetic alphabet has been shown to be very helpful when used to teach children with hearing impairment to read and to speak.
The auditory and auditory-visual phoneme recognition audiometry video and audiotape are for both phoneme recognition testing, as well as auditory and speech training. The audiovisual capabilities of the videotape are especially helpful for children with cochlear implants. Therapists, teachers, and parents who follow a multisensory philosophy for hearing habilitation will find a phonetic alphabet and audiovisual recognition training very helpful for teaching, reading, and speech. (Readers may wish to visit www.journeytoliteracy.org.)
Speech Perception Index
Most patients appreciate being informed about their hearing problem and of ways to improve their understanding of speech. An instrument which helps to convey information to the patient is the Speech Perception Index (SPI). To determine a person’s SPI locate the patient’s Speech Reception Threshold (SRT) at the top of the SPI chart (Figure 6) and Phoneme Recognition Loss (PRL) at the side of the chart. To calculate the PRL, one must subtract the test score of either the “Quick Test” or “Inventory Test” from 100%. The number where the two lines intersect is the SPI. Two index scores may be obtained: 1) from auditory only, and 2) from auditory-visual. The location of the index figure will indicate the patient’s degree of impairment (ie, normal, slight, moderate, severe, or profound).

Figure 6. To determine a person’s Speech Perception Index (SPI), locate his/her speech reception threshold (SRT) at the top and phoneme recognition loss (PRL) at the side. The number where the two indices intersect represents the Speech Perception Index (SPI). The index is obtained with auditory and auditory-visual speech signals. The location of the index figure will indicate the client’s degree of impairment (ie, normal, slight, moderate, severe, or profound). Revised by Duffy (1987).
The phoneme recognition inventory test scores in Figure 2 will be used to illustrate the use of the Speech Perception Index of a hypothetical patient. With an auditory unaided and aided PRL of 24% (100-76=24) and an auditory unaided SRT of 70 dB, the SPI will be 100 (severely impaired). When aided, with a SRT of 35 dB and with a PRL of 24%, the SPI will be 65 (moderately impaired). With an aided auditory-visual PRL of 7% and an aided SRT of 35 dB, the SPI will be 45 (slight loss).
Most patients will be impressed with this evidence of the benefits obtained through amplification.
Improving Speech Perception and Discovering Counseling Needs
As a result of phoneme recognition testing, the tester and the patient will have discovered the phonemes that the patient has not recognized in the words that were presented. Phonemes that are not recognized—even though they may fall within the speech spectrum area of audibility for the patient—may eventually become recognizable to the patient through the process of auditory learning.
Auditory learning takes place when the patient becomes aware of the acoustic characteristics of a phoneme which makes it distinguishable from other speech sounds. This ability to distinguish between phonemes can often be acquired by a motivated hearing-impaired individual if he/she becomes an attentive listener and observer in speech communication situations. This is especially true if the person is aware of the speech sounds that are the most difficult for him/her to perceive. Sometimes the audible features of certain phonemes are insufficient for the patient to recognize; however, when transition frequencies, visual cues, and contextual cues are present, word recognition is achieved.
The aided responses from tonal soundfield audiometry may show that certain phonemes—particularly the unvoiced consonants—are inaudible to the patient. Fortunately, in the production of many of these difficult-to-hear speech sounds, visually discernable lip postures and lip movements provide the cues that make these phonemes recognizable. An attentive listener who watches the speaker’s lips can usually learn to associate visual cues with auditory and contextual cues, with the result that the speech signal becomes intelligible.
Patient Support
The following are a few suggestions in support of the patient’s efforts to improve his/her speech perception ability:
• Before the widespread use of hearing aids, lipreading enjoyed an acceptance that no longer exists because lipreading is a very poor substitute for hearing. However, the value of lipreading as a supplement and complement of hearing has been amply demonstrated by many hearing-impaired persons who find that they “hear” better when they can see the face of the speaker.
• The results of the phoneme recognition tests should be explained to the patient. The patient should be told which phonemes he/she can hear through amplification and which speech sounds may require the visual cues that lipreading provides. A copy of the patient’s test response form which shows the omissions and substitutions, as well as the correct responses, can be shown to the patient. The patient who is eager to improve his/her speech perception ability and who wishes to pursue a self-help program will benefit from this information.
• It should be suggested that the patient enlist the assistance of a family member or friend to help him/her to recognize words that contain sounds that are difficult for them to hear. This can be done by having the family members read to the patient. Words, phrases, sentences, and paragraphs —without and with visual cues—should be presented. Naturally, sounds that are inaudible to the patient, even with amplification (eg, unvoiced consonants) will require the assistance of visual or contextual cues for recognition. Have the patient return at a designated time (eg, a month or more depending upon the needs of the patient) for re-testing phoneme recognition and for follow-up instruction and encouragement as required. Have the patient return on a regular basis to re-evaluate and service the hearing aids and to re-evaluate the patient’s auditory and auditory-visual phoneme recognition ability.
Friendly, competent, respected dispensing professionals should be thought of by their patients as professionals, not as merchants. Satisfied patients, who trust their dispensing professional, will—through the “grape vine”—make many referrals. What better way to “market” hearing rehabilitation and the hearing care profession?
Authors’ Note: A manual discussing the above hearing rehabilitation protocol in more detail, copies of “Quick” and “Inventory” test forms, as well as the videotape and audiotape of all tests, can be obtained from the Speech for The Deaf Foundation Inc, 41 Amherst Rd. Port Washington, NY 11050, (516) 767-2549; email: [email protected].
Correspondence can be addressed to HR or John K. Duffy, PhD (see address above); email: [email protected].

|