By Michael Piskosz, MS
BZZZZ! WHOOSH! FZZZZ! RING! No, it’s not Superman blazing by to the rescue, but rather some of the more common descriptions of tinnitus.
And just as there has been a growing popularity of super hero movies taking over the big screen, tinnitus is also a growing trend in today’s world, affecting 10-15% of the overall population.¹ As hearing loss is increasingly identified and diagnosed, this trend is most likely to continue and grow, thereby putting tinnitus on the horizon of standard audiology practice. Still, many clinicians feel overwhelmed about tinnitus and what can be done to address it.²
By virtue of my position with a hearing instrument manufacturer, I have the opportunity to visit clinics all over the world. This has given me a broad perspective on the services hearing care professionals offer to their patients. Audiologists and dispensing professionals are typically very comfortable in the realm of audiologic diagnostics, hearing aid fittings, and follow-ups—after all, that’s what we’ve been trained in. However, when the conversation turns to tinnitus, I often see a look of confusion and uncertainty on many clinicians’ faces.
The world of hearing healthcare is changing. This evolution spans changes in hearing healthcare benefits and service delivery models to advances in hearing aid technology to what the future may hold in biologically based therapies for hearing loss, such as hair cell regeneration. The effects of any of these changes on our practices are unpredictable and out of our control to some degree. Therefore, being the experts in hearing care and the application of several tools that directly benefit those with tinnitus, it would appear that tinnitus services are a unique and valuable offering—an extremely useful addition to a practice or clinic.
In particular, it makes good sense for the audiologist and dispensing professional to lead the way in tinnitus management. One reason is that, even though the exact cause of tinnitus is still unknown, we do know that the auditory system plays a significant role in tinnitus perception. Second, regardless of what type of management protocol is used, sound therapy (including hearing instrument amplification alone) almost always plays a vital role in the outcome. And, because of the importance of sound therapy, the diverse professional disciplines typically involved in tinnitus management tend to agree that audiologists should play a fundamental or even primary role on the care team.

|
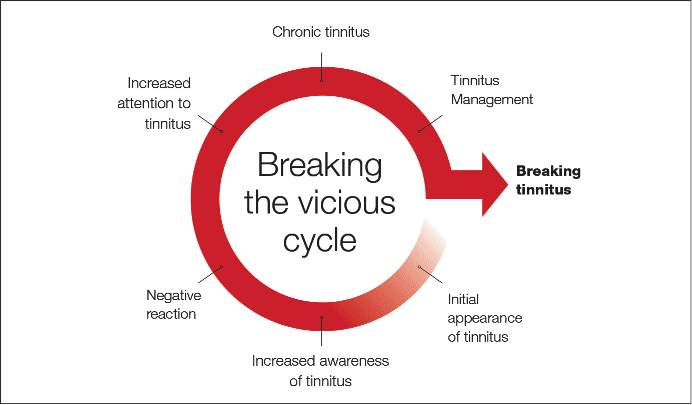
| Figure 1. The vicious circle of tinnitus. (click to enlarge) |
Although audiologists should be at the forefront of tinnitus management, a multidisciplinary team can be very useful in helping to break the vicious cycle that many tinnitus sufferers fall victim to (Figure 1). Finally, considering that approximately 80% of tinnitus sufferers also have some form of hearing loss, it justifies the crucial role audiologists and dispensing professionals play in tinnitus management.³
Where Do I Start?
The comment I most frequently hear from clinicians in regard to helping tinnitus patients is “Where do I start?” The quick and easy answer to that question is “Education.”
The biggest hurdle clinicians face when it comes to tinnitus management is that most of us do not have the knowledge base to help these individuals. We typically don’t receive enough tinnitus training from our university curriculum, and many don’t know where to turn to get this knowledge once they are working clinically. One way to learn the first steps to incorporate tinnitus management into your practice is at one of the numerous tinnitus conferences offered annually.
The University of Iowa holds an annual conference (June 14-15 in 2013), and the Tinnitus Practitioners Association (TPA) holds multiple conferences yearly that offer practical clinical information that can easily be incorporated into your clinic right away. On the other hand, the Tinnitus Research Initiative (TRI) conference offers a yearly conference that involves higher-level neuroscience applications of tinnitus, which help identify sites of causation and future research involved with tinnitus.
This article also aims to provide guidance and direction on how to incorporate tinnitus into your practice, but should be considered only as an outline of first steps, as further education from your side will be necessary to successfully incorporate tinnitus services fully.
The Role of You and Your Clinic
The ultimate role of the hearing care professional in tinnitus management is to provide the patient with guidance through professional knowledge. The information that should be covered with the patient includes, but is not limited to: causes, effects on life, solutions, realistic expectations, and appropriate use of sound therapy, which may or may not include the use of hearing instruments.
Although the primary responsibilities fall on the hearing care professional, tinnitus management starts at the first point of contact. In many cases, this can be clinic staff. It is worthwhile to also have your staff trained on basic tinnitus knowledge (they can join you at tinnitus courses/trainings), so that they can ask appropriate questions for appointments and referrals. Having your staff understand basic tinnitus terminology can help you collect valuable patient information prior to their first visit. Clinic staff also can be responsible for sending out tinnitus information to the patient before the appointment, so the patient can arrive with a fair and realistic expectation of your services.
It is also important to let the community know about the tinnitus services you provide. Many of your referral sources and colleagues in other professional disciplines may not be up-to-date on the latest management options for tinnitus. Offering professional educational seminars to the community is a good way to educate your referral network about tinnitus.
In addition, consumer seminars can be valuable, as this can help both the local community understand tinnitus better, while highlighting your expertise and clinical services.
Successful Tinnitus Management
The most concrete way to determine successful tinnitus management is through the use of questionnaires, which provide a quantitative means of monitoring the perception of one’s tinnitus. A number of questionnaires are available, including the Tinnitus Handicap Inventory (THI), Tinnitus Reaction Questionnaire (TRQ), Tinnitus Functional Index (TFI), and Tinnitus Handicap Questionnaire (THQ). Each questionnaire differs in its sensitivity to the different aspects of tinnitus. Although it is essential to incorporate a questionnaire into your tinnitus protocol, it should not be the only measure to monitor the status of one’s tinnitus perception. Subjective comments are very important, as this offers the patient a platform to express their thoughts regarding tinnitus.
In addition to objective measures of tinnitus perception, there are other guidelines that are recommended for successful tinnitus management. Keep the following guidelines in mind when incorporating tinnitus services into your practice:
Structured, but flexible. Goals and milestones within achievable time frames should be established, but understand each person experiences tinnitus differently.
Patience. Treatment takes time; not everyone will proceed at the same pace. Take on what you can handle in the context of your clinic’s resources.
Attentive/sympathetic. Don’t assume the patient knows what you know. Listen to them and how they are explaining their experiences. Tinnitus dramatically affects some people’s lives.
Encouraging, but truthful. There are things that can be done to help treat tinnitus, but it is also important to set realistic expectations.
Use of outcome measures. Ways to monitor change/progress over time are essential. These can include pre- and post-questionnaires, and changes in loudness or minimum masking levels (MMLs).
Start small. Scale goals and tasks appropriately for where the individual is in their treatment. For example, understanding how to successfully use sound in their environment could be one of the first steps. The patient should assume the responsibility at some point.
Confidence. A successful treatment plan is a plan you are comfortable and confident in. Remember, you are the professional.
Network. It is important to have a strong working network of specialists. Not all aspects of tinnitus are audiology-related. Cultivate relationships with other professionals such as psychologists/psychiatrists, ENTs, and massage therapists.
Continuous learning. New tinnitus-related research and products emerge every year. Keep yourself updated and develop a protocol with flexible solutions. Knowledge about other sound tolerance issues (ie, misophonia/phonophobia and hyperacusis) is also important.2,3
Finally, one of the most vital aspects of successful tinnitus management is to establish a tinnitus protocol for your clinic. Having an established protocol allows you to have a structure in place that you can rely on when working with this population.
As each case of tinnitus is unique, making individualized modifications along the way will customize the management course for each individual. This is why it is important to be knowledgeable about the different approaches to tinnitus management, as one paradigm will not work for everyone. The most common approaches to tinnitus management are hearing instrument amplification (for those with hearing loss), Sound Therapy, Tinnitus Retraining Therapy (TRT), Progressive Tinnitus Management (PTM), Mindfulness-based Therapy, and Cognitive Behavioral Therapy (CBT). Yearly seminars/courses are offered to learn more about each approach to tinnitus management.
Establishing a Protocol
Establishing a protocol can be one of the more challenging tasks when incorporating tinnitus into your practice. A common concern among clinicians seems to be the perception that tinnitus patients require a lot more time than traditional hearing instrument patients. Without an established protocol, this can be true, as a lack of direction almost always results in wasting valuable time. But once you get comfortable working with tinnitus patients, the amount of time spent with these individuals can be similar to follow-up appointments for hearing instruments. Since a key component to tinnitus management is counseling, it is important to have direction and goals set for each appointment (see sidebar for a sample protocol).
Marketing and Cost for Services
One of the most important elements of any clinic is to create public awareness of the services that you offer. In general, the many people who struggle with tinnitus simply do not know what can be done, or who can help them. Incorporating tinnitus into your marketing plan can help create public awareness, while distinguishing you from your competitors who may not offer total hearing care services.
A good example of this is consumer seminars. Holding seminars that help explain to the public what tinnitus is and what can be done can prove beneficial in identifying yourself as the tinnitus leader in your community. These seminars also can be held for other professionals in your area, increasing your referral source.
In addition, since successful tinnitus management is largely about counseling, it is not uncommon to spend more time on the front end of a tinnitus management plan educating your patient. As you advance further into your protocol, and if the patient is progressing, the amount of counseling will most likely decrease, and more time will be spent on what they are doing to manage their tinnitus and how it is affecting their life.
Like any professional who offers a service, you should charge accordingly, as you are offering professional advice and help. It is not uncommon to spend 1 to 2 hours during an initial tinnitus consultation, gathering case history information, diagnostic information regarding the tinnitus (ie, pitch matching, loudness matching, minimum masking levels, and/or residual inhibition trials), and reviewing sound therapy options if applicable. A fee that you feel is appropriate should be charged for this time. Frequently, if a patient decides to purchase sound therapy instruments (eg, combination units, neurostimulators, etc), this fee can be incorporated into the cost of the instruments. Other considerations should include follow-up visits, batteries, and any accessories, such as wireless streaming devices.
Another question that often arises is whether services should be bundled or charged separately. This is up to you, of course, based on how your clinic operates. But many clinicians feel that a bundled charge for tinnitus services is more effective at having patients commit to the protocol, rather than charging for services separately as you go. An example of a bundled package can include a set number, or unlimited, clinic visits for 12 months that include tinnitus counseling and fine-tuning adjustments of any instruments. The package you offer might differ according to the approach you take, such as TRT versus traditional masking. This bundled charge would be on top of the cost of the instruments.
Bundling is something you see in everyday consumerism, such as extended warranties, home communication/entertainment packages, and travel packages to name a few. Ultimately, you should charge for your services in a way that is consistent with your clinic’s practices and that you are comfortable with. A good resource on this subject is the ASHA website at: http://www.asha.org/Practice/reimbursement/privateplans/Bundling-Versus-Unbundling
Waiting for Our Superhero
| Resources |
|
University of Iowa Tinnitus Conference |
As we have discussed, many people struggle living with tinnitus and more people are being identified every day. It is important—not only for the quality of life of your patients but also for the long-term health of our profession—that we do more to incorporate tinnitus services into our practices.
There are courses and conferences that provide deep insight on how to work with tinnitus patients and how to make these services a fundamental part of your clinic. We as hearing care professionals should strive to do more when it comes to tinnitus. Individuals battling tinnitus need our help, and until we find our Superman of tinnitus, we are the best hope for people suffering from it.
References
1. Davis A, Refaie AE. Epidemiology of tinnitus. In: Tyler R, ed. Tinnitus Handbook. San Diego: Singular Publishing Group; 2000:1-23.
2. Tyler RS, Haskell G, Gogle S, Gehringer A. Establishing a tinnitus clinic in your practice. Am J Audiol. 2008;17:25-37.
3. Vernon JA. Introduction. In: Vernon JA, ed. Tinnitus Treatment and Relief. Needham Heights, Mass: Allyn & Bacon; 1998:xiii-xvii.
4. Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. Boston: Cambridge University Press; 2004:276.

|
Michael Piskosz, MS, is board certified in audiology and a member of the ReSound Global Audiology Team in Glenview, Ill, where he develops audiology-related training materials based on research and development. CORRESPONDENCE can be addressed to the author at: [email protected] |
|
Appendix
|
|
The following is an example of a tinnitus protocol: Step 1: Tinnitus Consultation 1) Case history: Collect a thorough and detailed case history. • Demystify the nature of tinnitus by providing education regarding possible causes, etiologies, and reassurance that tinnitus is a “real” condition that is treatable, but not yet curable. Address any sound tolerance issues, such as hyperacusis, misophonia, or phonophobia. Step 2: Introducing Sound Stimulation This can take place in the same visit as the Tinnitus Consultation (Step 1) in some instances, or can be done at a separate visit. 1) Follow the fitting instructions of the preferred sound solution for tinnitus sound generators (TSG), sound stimulators, etc. Note: Alternatively, you can start by using just the hearing instrument amplification for individuals with treatable hearing loss. Step 3: Follow-up Visit 1 Starts about 2 weeks after first fitting. 1) Discuss subjective comments/feedback from the patient relative to:
2) Provide tinnitus counseling to:
3) Make necessary adjustments to TSG, but only if required. This may include:
Step 4: Follow-up Visit 2 About 4 weeks after first fitting. 1) Discuss subjective comments/feedback from patient.
2) Provide tinnitus counseling. 3) Make necessary adjustments to TSG, but only if required. This may include:
4) Re-administer any questionnaires given at the start of treatment to monitor status of tinnitus perception. Step 5: Follow-up Visit 3, 4, and 5
1) Follow-up Visits 3, 4, and 5 should follow the same steps as Follow-up Visit 2, including post-measure questionnaires. More visits may be required for some individuals. Keep in mind this is just an example layout for a tinnitus protocol. Actual management steps and timelines may vary, and should be considered on a case-by-case basis and/or in concert with a multidisciplinary team. Many tinnitus patients may require considerably longer than 6 months of treatment (eg, 12 to 18 months),4 and severe cases may warrant referral. The take-home message is that it is important to have some structure for both you and the patient to follow. |
MORE ON TINNITUS can be found at:
MarkeTrak VIII: The Prevalence of Tinnitus in the United States and Self-reported Efficacy of Various Treatments, by Sergei Kochkin, PhD, Richard Tyler, PhD, and Jennifer Born (Nov 2011 HR)
Podcast interview with Drs Kochkin & Tyler: Changing Reactions to Tinnitus, by Laurence McKenna, PhD, and Gerhard Andersson, PhD (Aug 2007 HR) (available online soon)