Tech Topic | November 2014 Hearing Review
By Melanie Herzfeld, AuD, Enza Ciurlia-Guy, MClSc, AUD(C), and Robert Sweetow, PhD
The results from this clinical study strongly support the use of Widex Zen Therapy in tinnitus patient management. The data revealed substantial positive adjustment to tinnitus, as measured by the TFI and THI, evident within the first 2 months of treatment, with further (albeit not statistically significant) changes occurring through 6 months. The average (mean) reduction in THI scores was 30 points (23 points after only 2 months) and was 28 points in TFI scores (25.5 points after only 2 months). Additionally, 74% and 75% of subjects achieved clinically significant changes in their THI and TFI scores, respectively.
Previous reported investigations of hearing aids containing fractal tones1-6 have yielded favorable results in reducing the tinnitus annoyance or handicap for patients with significant tinnitus. It appears that a combination of fractal tones (generated by hearing aids), amplification, and counseling have great potential for tinnitus patient management.
Derived from these findings and subsequent research, Widex introduced a new tinnitus management approach called “Widex Zen Therapy” in 2012.7 The overall objective of Widex Zen Therapy (WZT) is to ensure that the tinnitus does not negatively impact the patient’s quality of life. Because it is well accepted that distress related to tinnitus is highly correlated with hearing loss, negative emotions, fear, and stress, WZT incorporates four key components:
1) Counseling, both instructional and adjustment-based, to educate the patient and assist the limbic system to modify the negative interpretation of the tinnitus via cognitive and behavioral intervention;
2) Amplification to stimulate the ears and brain in order to minimize increases in central activity (overcompensation) and maladaptive cortical reorganization;
3) Zen acoustic options include fractal tones, a novel, proven acoustic stimulus that sounds somewhat like wind chimes, delivered dichotically in a discreet, inconspicuous, and convenient manner, designed to both relax and provide acoustic stimulation, broadband, and/or filtered broadband noise;
4) Relaxation strategy program, highlighted by relaxation exercises and sleep management strategies.
The appropriate components constituting the therapeutic intervention are tailored for each individual in accordance with the audiologic evaluation and the patient’s reaction to the tinnitus. The more severe and negative the tinnitus reaction, the more components listed above will be added in the individualized program.
The objective of this multi-site clinical cohort study was:
1) to evaluate the effectiveness of WZT over a period of 6 months for subjects with significant tinnitus (with or without measurable hearing loss), and
2) to investigate how subjects employ the hearing aids and the acoustic (fractal tones or filtered noise) options.
Methods
Two tinnitus clinics participated in the data collection (Hearing and Tinnitus Center Tinnitus Clinic in New York and Canadian Tinnitus and Hyperacusis Centre in Whitby, Ontario, Canada). All subjects participating in the study met the following criteria: medical clearance/medical management prior to treatment; clinically significant level of tinnitus-related disturbance (Tinnitus Handicap Inventory8 score greater than 18); normal hearing or pure-tone average hearing loss no greater than 70 dB HL; adequate cognitive comprehension to engage in WZT; manual dexterity conducive to handling the hearing/tinnitus devices; capability to pay for the tinnitus therapy; and availability to attend follow-up sessions for up to 6 months post hearing aid fitting. All participants signed an informed consent form.
Subjects were given a comprehensive audiologic and tinnitus evaluation by trained tinnitus clinicians at the two clinical sites. They completed the detailed Widex Tinnitus Intake Questionnaire, Tinnitus Handicap Inventory (THI),8 and Tinnitus Functional Index (TFI).9
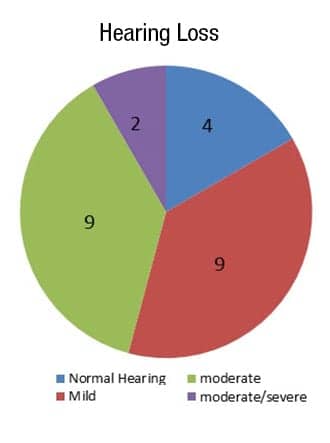
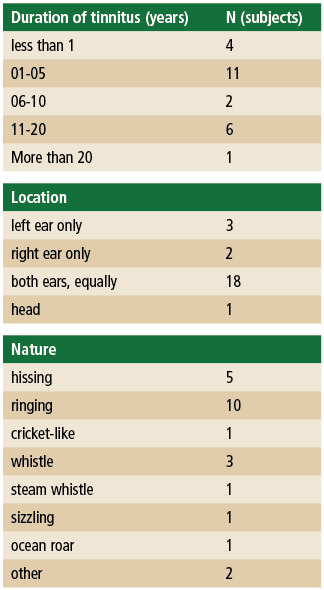
Participants. A total of 32 subjects were initially enrolled, but only 24 subjects completed the data collection. The other 8 subjects kept the hearing aids but were excluded from the final data analysis because they did not return for the 6-month follow-up. Six females and 18 males (mean age 58, ranging from 29 to 80) participated. A total of 22 of the 24 subjects were first-time hearing aid users. Hearing losses ranged from mild to moderate-severe. Figure 1 shows the hearing loss distribution among subjects. Four subjects had normal hearing (defined as pure-tone average less than 25 dB HL).All subjects had significant tinnitus distress (THI >18) when they enrolled in the clinical study with a mean THI score of 51, ranging from 20 to 96. The mean tinnitus loudness was 6 (on a 10-point scale) and the tinnitus pitch was 7 (on a 10-point scale). Only 6 of the subjects indicated having received previous tinnitus management such as counseling, chiropractic adjustment, medication, dental treatment, Neuromonics,10 and hearing aids. Twenty of the 24 subjects reported having had tinnitus for more than 1 year, and 18 reported having bilateral tinnitus. The nature of tinnitus sound varied, but hissing and ringing were most often reported. The duration of tinnitus, location, and quality reported by the subjects are shown in Table 1.
Clinical procedure. Subjects participating in the study were patients who visited the clinics to seek tinnitus management. The initial Widex Intake Questionnaire, THI, TFI measures, and the clinician’s observation of the subjects were used to determine which components of Widex Zen Therapy were utilized during the treatment.
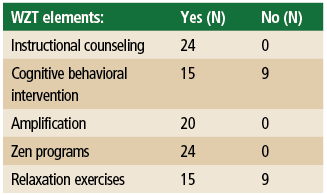
All subjects were provided with an explanation about Widex Zen Therapy and the treatment guidelines, which included Widex hearing aids, the proprietary Widex Zen program (consisting of fractal tones and/or noise), and comprehensive instructional counseling. In addition, adjustment-based cognitive behavioral intervention (explained below) and relaxation exercises were applied for those individuals demonstrating more severe negative reactions to their tinnitus. Table 2 shows the number of subjects receiving the various WZT components in the clinical trial.
Instructional counseling. All subjects received detailed instructional counseling related to the hearing loss and tinnitus. In addition, the relationship between impaired hearing and tinnitus perception, as well as the reasons why there is commonly an emotional connection established in the brain between the limbic system, autonomic nervous system, and the auditory cortex, was explained.
Instructional counseling was similar to that provided in Tinnitus Retraining Treatment (TRT)11 directive counseling. The objectives were to provide the patient with an understanding of the habituation process and to help the patient reclassify the tinnitus. For example, the instructional counseling addressed:
- The basic anatomy and physiology of the auditory (and central nervous) system
- Why the tinnitus is present (particularly when it is a normal consequence of having a hearing loss)
- What the logical course of the tinnitus might be
- How the limbic system affects the tinnitus perception and how the patient’s reaction impacts the ability to cope with or habituate to the tinnitus
Cognitive behavioral intervention. Because many clinicians feel instructional counseling alone is not adequate to address the emotional consequences of tinnitus, including fear, anxiety, and depression,12 WZT recommends adjustment-based counseling or Cognitive Behavioral Intervention (CBI) to help the patient identify barriers to achieving natural habituation. This intervention utilizes segments of the programs and tools used by psychologists and clinicians who provide comprehensive Cognitive Behavioral Therapy. However, CBI does not require the same intensive therapeutic approach, which would be beyond the expertise of many hearing care professionals and would require a greater time commitment than can be reasonably expected. During this phase, the clinicians help the patient identify the unwanted thoughts and behaviors hindering natural habituation, challenge their validity, and help the patient replace them with alternative and logical thoughts and behaviors.13 Basically, the intervention’s objective is to help the patient recognize that it is not the tinnitus itself that produces these beliefs, it is the patient’s reaction to tinnitus.
Amplification. All subjects were fit bilaterally with Widex Dream hearing aids with True Input Technology that remain undistorted at the input stage with inputs as high as 113 dB SPL. These instruments have wide dynamic range compression (WDRC) with compression thresholds as low as 0 dB HL, adaptive multichannel directional microphones, noise reduction, active feedback cancellation, inter-ear communication, and data logging.
The choice of the particular model (which varied from the high end 440 to the entry level 110) was based on the individual patient’s needs and economic considerations. All of the hearing aids were programmed to have four memories; a “master” (amplification only) program, and three “Zen” programs, as explained below. The four normal-hearing subjects had their hearing aids programmed as if they had a 15 dB hearing loss in order to ensure audibility of the Zen programs. Subjects with hearing loss were instructed to use the devices during waking hours where hearing and communication were essential.
Zen programs. The Zen programs use fractal (Zen) tones that are generated by a semi-random recursive algorithm. The fractal tones are harmonically related but vary in tonality, intensity, or tempo over time. The tones (which sound somewhat like wind chimes) are generated while incorporating the properties of music that are proven to be most relaxing.1,2,7 Thus, they are meant to be pleasant and are not associated with music that the listener may hold in memory.
There are five Zen fractal tone styles available that vary in their tempo, pitch, dynamic range, and chord. In addition, fine-tuning adjustments of each style can be made to its pitch, tempo, and volume by the clinicians. Each Zen setting was programmed in accordance with the hearing loss (based on the Sensogram) to assure audibility of the tones. While most subjects chose to have the clinician create individualized changes in their Zen programs, as will be explained in the Results section below, the recommended Zen programs for subjects with hearing loss were as follows:
- Zen Program A utilized the “Aqua” setting that has proven to be the most popular fractal tone style. These tones are characterized by a relatively low default pitch, major chord tonality, restricted dynamic range, and slow tempo, along with the microphone placed in the “on” position;
- Zen Program B used “Aqua” with the microphone set to either “on” or “off,” depending on the subject’s preference, and also included a filtered broadband noise; and
- Zen Program C utilized only the noise with the microphone “on.” For the four normal-hearing subjects, all Zen programs were programmed with the microphone “off.”
Subjects were instructed on hearing aid use, including how to access the various Zen programs and how to adjust the volume. They were told that the fractal tones should be audible, but soft enough to not interfere with conversational speech. They were further advised to avoid frequent volume changes and to use the Zen programs as much as needed for tinnitus and relaxation management and to avoid silence when possible. Zen Programs B and C were only recommended if the subjects experienced periods where the tinnitus was very bothersome.
Relaxation strategy program. The use of relaxation exercises was given to patients to break the vicious cycle of tinnitus and stress. Therefore, each patient with negative reactions to tinnitus or who demonstrates the need for stress reduction was prescribed and taught relaxation technique such as progressive muscle relaxation, deep breathing, and guided imagery.14
Outcome measures. The TFI and THI were administered as the principal measurement instruments in the study. Tinnitus measures and hearing aid data logging information were collected at baseline, 2 and 6 months.
Results
The mean baseline THI was 51 (range 20 to 96), while the final THI was 21 (range 0 to 54). The mean improvement was 30 points. This difference is statistically significant on the Friedman’s Two–Way Analysis of Variance repeated measures (p < 0.001). Moreover, a mean 22 point statistically significant improvement from the baseline was shown as early as 2 months from the baseline visit (p < 0.001). Although the THI continued to improve between the 2nd and 6th month follow-up visits, the difference was not statistically significant (p > 0.05).

Figure 2. Mean Tinnitus Handicap Inventory (THI) and Tinnitus Functional Index (TFI) scores at baseline, 2 and 6 months. Error bars represent standard error.
The mean TFI baseline score was 53 (range 20 to 82), while the final TFI mean score improved to 25 (range 0 to 62). The mean improvement was 28 points. A repeated-measures ANOVA showed that visit was a significant factor (F [2, 46=26,04; p < 0.001). Post hoc analysis with adjustment for multiple comparisons using a paired-samples t-test also showed significant tinnitus relief at the 2-month visit (p < 0.001) compared to the initial visit. No significant changes (p < 0.05) were seen between months 2 and 6. Figure 2 shows the data for both the THI and TFI.
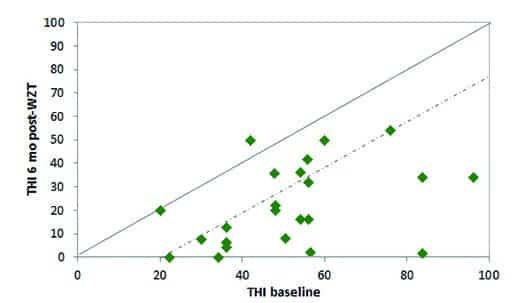
Figure 3. Individual subject Tinnitus Handicap Inventory (THI) baseline and 6 months post Widex Zen Therapy scores for 23 subjects (one subject was missing the THI at baseline). The solid line represents equivalent baseline vs final (post treatment) scores while the dashed line represents the 20-point benefit score considered clinically significant.
Individual subject scores for the baseline and 6 months after WZT are shown in Figures 3 (THI) and 4 (TFI). Note that the solid diagonal lines reflect equivalent pre- and post-scores. Symbols falling beneath this solid diagonal line indicate reduction in tinnitus handicap. The dashed line in Figure 3 represents the critical difference of 20 points reflecting clinically significant changes in the THI,8 and the dashed line in Figure 4 represents the critical difference of 13 points reflecting clinically significant changes in the TFI.9
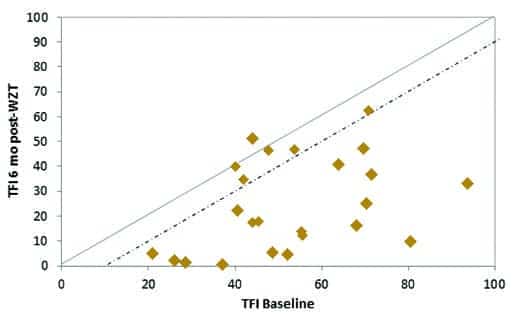
Figure 4. Individual subject Tinnitus Functional Index (TFI) baseline and 6 months post Widex Zen Therapy scores for the 24 subjects. The solid line represents equivalent baseline vs final (post treatment) scores while the dashed line represents the 13-point benefit score required for clinical efforts to be considered clinically significant.
Symbols falling below these diagonal dashed lines reflect clinically significant relief from tinnitus on these two scales. Inspection of individual subject data revealed that 74% of subjects obtained a clinically significant change in THI scores, and 75% of the subjects had clinically significant changes in TFI scores.
There were strong positive correlations (r = >.81; p = 0.001) found between TFI and THI for all the three visits (baseline, 2 and 6 months), suggesting that both subjective scales were sensitive, and quite equivalent, measures of improvement during the clinical trial. In addition, the degree of improvement (in terms of THI and TFI reduction) was slightly greater (though not statistically significant) for the subjects receiving the more comprehensive cognitive behavioral intervention and relaxation exercises.
Individual Preferences and Wearing Habits
A secondary objective of this study was to ascertain individual preferences and wearing habits for the hearing aids and programs. Figure 5 shows the choice of Zen A, B, and C programs selected at the initial fitting.

Figure 5. Choice of styles and microphone settings for Zen A, Zen B, and Zen C programs at the initial fitting.
The majority (80%) of subjects selected “Aqua style with microphone on” as their Zen A program. About two-thirds (65%) of the subjects selected “Aqua + microphone off” as their Zen B program. All subjects selected “noise-only with microphone on” as their Zen C program.
Data regarding the subjects’ use of the devices was collected at the two follow-up visits. The mean use of the hearing aids, (including amplification and Zen programs) recorded at the 2-month visit was 6.7 hours/day, and the mean use time recorded at the final session was 7.8 hours/day. A repeated-measures ANOVA indicated this difference was not statistically significant (p>0.05).
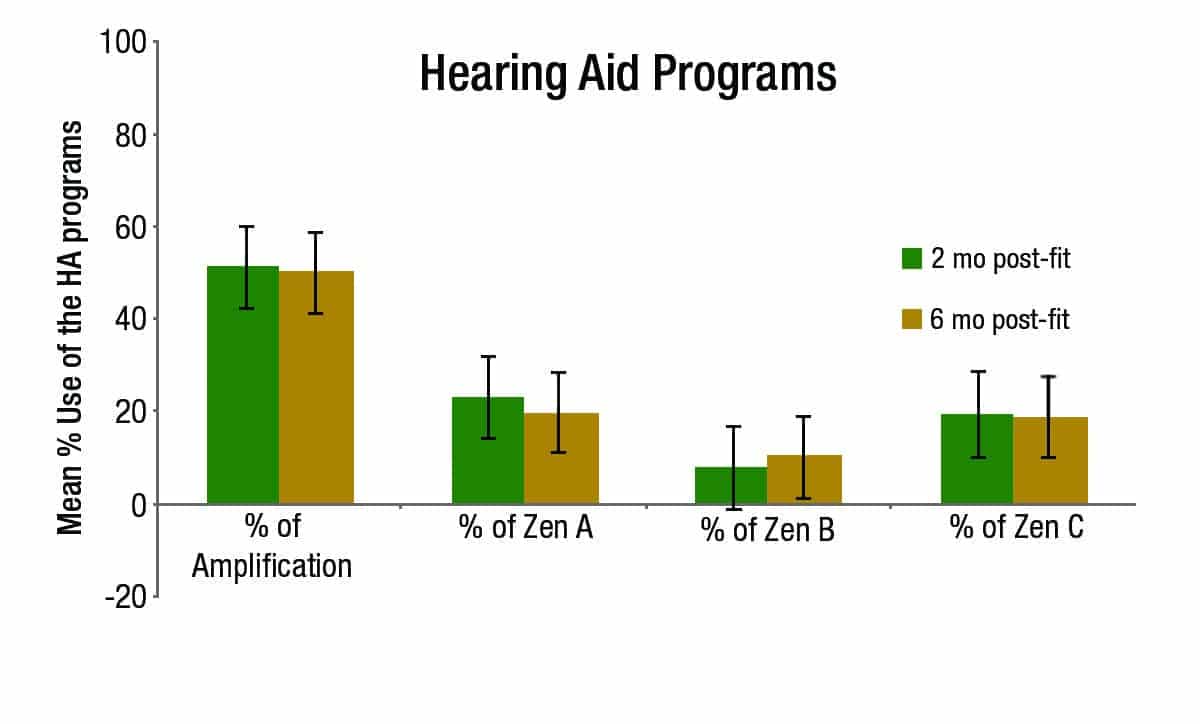
Figure 6. Percentage (time) of use of amplification only (Master program), Zen A, Zen B, and Zen C at the 2 and 6 month visits. Bars represent standard error.
Figure 6 shows the mean percentage of time use for amplification versus the three Zen programs. The average use of amplification only (the Master program) was 50%, and the average use of the three Zen programs combined was 50% also. This number remained quite similar throughout the study, based on a repeated-measures ANOVA (p > 0.05). In addition, data logging revealed that the Zen A and Zen C programs were used more frequently than the Zen B program. No statistical difference was seen for the use of Zen A between the two follow-up visits (p > 0.05); however, the mean use of Zen A decreased slightly by the second visit (from 23% to 20%). The mean use of Zen B increased slightly from 8% to 10% between the two follow-up visits, although a repeated-measures ANOVA showed no statistical difference between the two visits (p > 0.05). The mean use of Zen C program was 19% throughout the study. No statistical difference was seen for the use of Zen C between the two visits (p > 0.05).
Discussion
This study was the first to investigate the efficacy of full clinical employment of Widex Zen Therapy including its four key components (amplification, instructional and adjustment-based counseling, Zen fractal tones and/or noise, and relaxation exercises). The data revealed substantial positive adjustment to tinnitus (as measured by the TFI and THI) evident within the first 2 months of treatment, with further (albeit not statistically significant) changes occurring through 6 months. The average (mean) reduction in THI scores was 30 points (23 points after only 2 months) and was 28 points in TFI scores (25.5 points after only 2 months). All of these differences were both statistically and clinically significant.
Additionally, 74% and 75% of subjects achieved clinically significant changes in their THI and TFI scores, respectively. While other tinnitus treatments have reported similar success,16 the speed in which the WZT treatment achieved these changes is particularly impressive and vital, considering the importance of early success in maintaining motivation for tinnitus patients.
Although it is not possible to determine the relative contribution of each WZT component to the reduction of tinnitus handicap and quality of life improvement, it is interesting to note that the degree of improvement (in terms of THI and TFI reduction) was slightly greater (though not statistically significant) for the subjects receiving the more comprehensive cognitive behavioral intervention and relaxation exercises. It is also relevant to note that WZT is one of the few current tinnitus treatments utilizing amplification in addition to other sound therapy options. Given the high prevalence of hearing loss (often too mild to clearly warrant the necessity for hearing aids), the benefit of using amplification is an added value.
Conclusions
The results from this clinical study strongly support the use of Widex Zen Therapy in tinnitus patient management. This individualized comprehensive approach combining counseling (instructional and adjustment-based cognitive behavioral intervention), amplification, fractal tones and/or noise, and relaxation strategies was highly effective in reducing tinnitus handicap in a short period of time, with improvements apparent through at least the 6-month duration of this investigation.
Future clinical studies would be useful to lend support to these findings and to determine the longer-term efficacy of this treatment. In addition, investigations focusing on and delineating the individual components of WZT would help understand how each component contributes to the process.
Disclosure
Co-author Dr Robert Sweetow is a part-time paid consultant for Widex.
References
1. Sweetow R, Sabes JH. Effects of acoustic stimuli delivered through hearing aids on tinnitus. J Am Acad Audiol. 2010;21:461-473.
2. Kuk F, Peeters H, Lau CL. The efficacy of fractal music employed in hearing aids for tinnitus management. Hearing Review. 2010;17(10):32-42. Available at: https://hearingreview.com/2010/09/the-efficacy-of-fractal-music-employed-in-hearing-aids-for-tinnitus-management
3. Herzfeld M, Kuk F. A clinician’s experience with using fractal music for tinnitus management. Hearing Review. 2011;18(11): 50-55. Available at: https://hearingreview.com/2011/10/a-clinicians-experience-with-using-fractal-music-for-tinnitus-management
4. Sekiya Y, Takahashi M, Kabaya K, Murakami S, Yoshioka M. Using fractal music as sound therapy in TRT treatment. Audiology Online, Article#11623 [March 2013]. Retrieved from: http://www.audiologyonline.com
5. Zubizarreta A, Zubizarreta AF, Jeppesen AK, Caporali SA. Effects of amplification, fractal tones and noise in tinnitus management. Poster presented at: American Academy of Audiology annual convention, Boston, April 2012.
6. Skellgaard PH, Kristensen AP, Caporali SA. Effects of counseling, amplification and sound stimulation in tinnitus management. Poster presented at: Tinnitus Research Initiative annual meeting, 2013.
7. Sweetow R, Jeppesen AMK. A new integrated program for tinnitus management. Hearing Review. 2012;19(7):20-26. Available at: https://hearingreview.com/2012/07/a-new-integrated-program-for-tinnitus-patient-management-widex-zen-therapy
8. Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122:143-148.
9. Meikle MB, Henry JA, Griest SE, Stewart BJ, Abrams HB, McArdle R, Myers PJ, Newman CW, Sandridge S, Turk DC, Folmer RL, Frederick EJ, House JW, Jacobson GP, Kinney SE, Martin WH, Nagler SM, Reich GE, Searchfield G, Sweetow R, Vernon JA. The Tinnitus Functional Index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012;33(2):153-76.
10. Davis PB, Wilde RA, Steed LG, Hanley PJ. Treatment of tinnitus with a customized acoustic neural stimulus: a controlled clinical study. Ear Nose Throat J. 2008;87:330-339.
11. Jastreboff P, Gray W, Gold S. Neurophysiological approach to tinnitus patients. Am J Otol. 1996;17(2):236-40.
12. Wilson PH, Henry JL, Andersson G, Hallam RS, Lindberg P. A critical analysis of the directive counseling as a component of tinnitus retraining therapy. Brit J Audiol. 1998;32:273-286.
13. Sweetow R. Cognitive aspects of tinnitus patient management. Ear Hear. 1986;7(6):390-396.
14. Widex Zen Therapy Manual: Managing the Effects of Tinnitus. Lynge, Denmark: Widex A/S; 2012.
15. Davis PB, Wilde RA, Steed LG, Hanley PJ. Treatment of tinnitus with a customized acoustic neural stimulus: a controlled clinical study. Ear Nose Throat J. 2008;87:330-339.
16. Henry JA, Schechter MA, Nagler SM, Fausti SA. Comparison of tinnitus masking and tinnitus retraining therapy. J Am Acad Audiol. 2002;13(10) [Nov-Dec]:559-581.
CORRESPONDENCE can be addressed to Melanie Herzfeld at: [email protected]