By Douglas L Beck AuD, F-AAA, CCC-A
Jane Madell, PhD, F-AAA, CCC-A/SLP, LSLS, Cert AVT, is an audiologist, speech-language pathologist, and LSLS auditory-verbal therapist who has garnered a wide range of experience in her more than four decades in pediatric audiology. Recently, she and Joan Hewitt, AuD, designed the LMH Test to improve monitoring of hearing and listening ability for children with hearing aids and cochlear implants. Here, Douglas Beck, AuD, interviews Dr Madell about how the LMH Test is being used, as well as the concerning lack of audiology care for certain older adults with hearing and listening problems.
Douglas L Beck: Hi, Jane! Thanks for your time today!
Jane Madell: Hi, Doug. Thanks for the invitation.
Beck: Although I’d like to cover all matters in pediatric audiology, let’s focus today on a few of the most topical and pressing issues. For example, I know when we last spoke, in February 2022, the LMH test was just gaining traction and a lot of attention. Can you review the origin of the LMH test and its application?
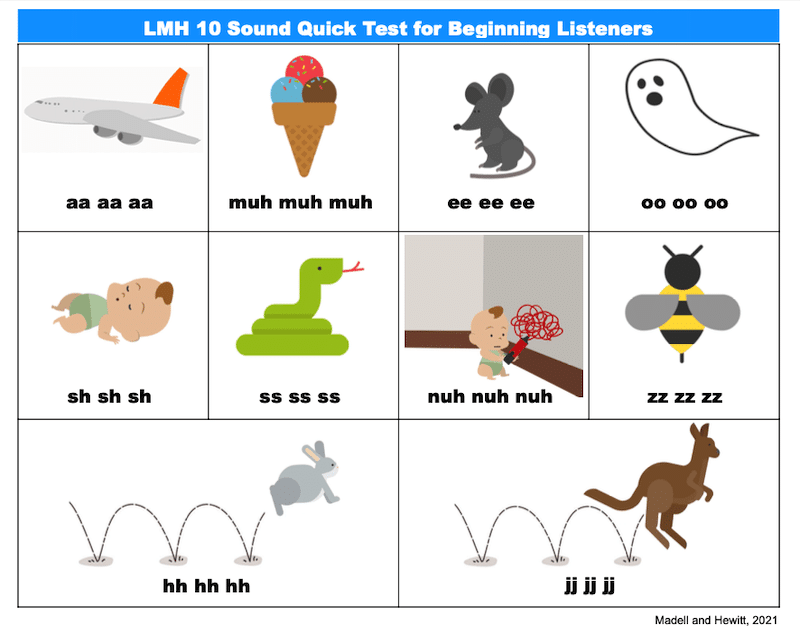
Madell: I would be delighted! The LMH Test was designed by Joan Hewitt and me for daily monitoring of the child’s hearing and listening ability. LMH is an acronym, and it stands for The Ling-Madell-Hewitt test or the Low-Mid-High frequency test. It can be used by the schoolteacher, school nurse, parents, and others to assure that the child wearing their technology is doing well in the left ear, the right ear, and binaurally.
Beck: And if we go back a few decades, prior to your development of the LMH, of course we had the Ling Six Sound Test. Can you talk about how the LMH evolved from the Ling 6 sounds?
Madell: Dan Ling, PhD (1926-2003), was a speech scientist and an AV therapist. He originally created the 5-sound test, and that eventually became the Ling Six Sound Test. The 6-Sounds Test was very useful to monitor speech perception using real-world sounds of speech. When Dan created the test, it was generally for children with hearing loss and hearing aids. In 2023, the test can be used for children with hearing aids, cochlear implants, and other technologies. However, the Ling Six Sound Test did not measure all the sounds of speech. It covers a few consonant bands but not a lot of information about the second and third formant bands, which we now know are critical for consonant differentiation.
Joan Hewitt and I studied this and decided to add four more consonants to provide a more comprehensive spectrum, and so the LMH was born. The LMH includes low, middle, and high frequencies (LMH) and conveniently also stands for Ling, Madell, Hewitt. We added in the sounds of /n/, /h/, /z/ and the first phoneme sound of the word “just,” which is phonetically transcribed as /d3/.
Beck: Excellent! And you and I have often discussed the value of functional assessments, going beyond sound-booth and threshold measures. Please tell me your thoughts on that.
Madell: When we test infants/children who are new to technology, we look for detection. Can they hear the target sound? As they get older and as we have more confidence in their fittings and programs, we need to make sure they can do more than hear. We want to make sure they can hear, learn, and listen in real listening situations.
Some children can repeat the stimuli/words, others point to pictures after the sound is verbalized (see illustrations below). Either is fine, but the key is we need to make sure they can hear, learn, and listen in each ear and with both ears, up close, and at a distance. This assures us that the child is doing well, and the equipment is working properly. If testing is binaural only, we cannot know if one ear (or one technology) is not working or performing well – and many times, the child won’t know or won’t be able to tell us. The way Joan and I see it, the audiologist should be responsible for teaching parents to develop the skills to do the technology screening on their own at home and reporting findings to the clinicians.
Beck: So just to reiterate, the parent or teacher vocalizes each of the 10 sounds while the child is wearing just their right technology, and then the same with just the left technology, and then with both technologies. And I believe the parent or teacher needs to vary the presentation order so the child doesn’t start to learn the order of the words, and it’s recommended to do an up-close and a distant test?
Madell: Exactly. And to be sure the information gathered is used efficiently, the parent needs to write down which sounds the child did not get correct, and in which presentation mode (left, right, both), so the audiologist has a better idea as to which sounds need to be addressed via programming or other protocols. And it’s very important to perform the test a few feet away from the child, to make sure the child can perceive the sounds from a distance, which might represent the classroom or other typical listening environments. We recommend sending the information directly to the audiologist and the educational or other multi-disciplinary healthcare team, so everyone is in sync and working toward the same goals and maximal communication.
Beck: I want to encourage readers to visit www.janemadell.com to get more information about the LMH test in English and in Spanish and to learn more about its history and how to use it. Jane, I think the whole profession thinks of you as one of the leading pediatric audiologists of all time, but I wonder if we might change the subject and talk about some issues at the other end of the spectrum—adult audiology issues.
Madell: Absolutely.
Beck: In my recent article in The Hearing Review on hospice and hearing healthcare, I note that despite my appreciation and admiration for hospice facilities and their professional caretakers, they don’t typically address the hearing and listening needs of their patients, the majority of whom have hearing and listening problems. In fact, when one signs up for hospice services, their care is primarily directed to pain relief and comfort, and that’s fine and appropriate. However, there is a big miss here. When people approach the last few months of life, particularly with chronic and worsening diseases, it seems obvious that their communication ability is of maximal importance. Yet it is left up to the patient and perhaps their loved ones to manage their communication needs.
Madell: This is a major problem, and thanks for asking about this. Yes. It’s not only hospice, but senior living centers, skilled nursing facilities (SNFs), nursing homes, and most places where older adults go for care and to have their basic needs met—there is no audiology. Oddly, in many SNFs (and other facilities) they offer speech language pathology services, which is great, but in general, the SLP hasn’t even done a hearing screening, and so I wonder how they know what the patient can perceive?
Beck: Right. You’ve hit upon a major issue, too. SLPs doing language or speech therapy without benefit of a hearing or cognitive assessment. Dr. Kathy Dowd at The Audiology Project has been a patient advocate for years addressing this and similar problems and she has written and spoken about it often. How can anyone do speech or language therapy without a comprehensive audiometric evaluation to demonstrate what the patient can hear and process? How can anyone offer language therapy without a cognitive screening to see how the patient is processing information?
I know many professionals think they can tell when a patient has hearing loss, but let’s face it, unless it’s a severe-to-profound hearing loss, no, they can’t. Most American adults (one-third by age 65 years, two-thirds by age 75) have hearing loss by the time they enter a care facility. And so, without a comprehensive audiometric test, the SLPs are just guessing, and that’s not in the patient’s best interest. Of course, some healthcare professionals and much of the public believe that if a patient passes silly tests like a whisper test or a watch ticking test, that the patient must have normal hearing and listening skills—which is most often simply not the case.
Madell: I agree. When my father-in-law was dying in hospice, he was having an extraordinarily difficult time communicating with family and staff. I bought him a portable, battery-driven personal amplifier with headphones, similar to a PocketTalker, but I purchased it at a local electronics store. It made all the difference in the world to him. It seems to me these facilities could have a few of those devices around and even if they’re not able to provide professional hearing services, maybe they could provide a few assistive listening devices to decrease the communication burden on the patient.
Beck: We all understand that bringing in specialists is not the goal of these facilities. However, if the goal is to assist the patient and help transition them into a more comfortable situation, the patient needs to hear and listen maximally, which, of course, should be a priority for these locations and professionals.
Naturally, like all of healthcare, it boils down to cost. Audiologists like you and me can be expensive, and many of these centers operate on shoestring budgets and a tiny profit, which they cannot afford to spend on specialists. And despite OTC, hearing aids can be a significant financial concern.
Nonetheless, it seems that if the hospice staff were to contact local audiologists, and if the local audiologists and dispensers were to reach out to the local hospice facilities, maybe they could offer an in-service on the basics of hearing, listening, communication strategies, and personal assistive listening devices (ALDs). ALDs could be purchased or leased as needed and as deemed most appropriate by the local professionals.
Madell: I think these are very good ideas and I hope the people reading this interview will act accordingly to help those unable to help themselves.
Beck: Jane, it is always a pleasure to speak with you and I am very appreciative of your time.
Madell: Thanks, Doug. I enjoyed it, too.
Douglas L. Beck, AuD, F-AAA, CCC-A, is an audiologist and consultant who serves on the Hearing Review editorial advisory board as the senior editor of clinical research and writes for multiple audiology, science, medical, and health-related professional organizations globally. He retired as vice president of clinical sciences at Cognivue Inc in June 2023. To learn more: www.douglaslbeck.com