Longtime cochlear implant users are reporting dramatic improvements in their hearing, thanks to new image-guided programming methods developed by Vanderbilt University researchers.
Using Vanderbilt’s patent-pending nonsurgical process, audiologists are able to fine-tune and customize cochlear implant programming, providing improved sound quality and clarity.
“Our automated image-guided programming method can dramatically improve a person’s hearing with a cochlear implant, even if implantation happened a long time ago. Study subjects have called it life-changing,” said Benoit M. Dawant, the Cornelius Vanderbilt Professor of Engineering and director of the Vanderbilt Initiative in Surgery and Engineering (ViSE). “This is an excellent example of collaborative effort between engineering and medicine that ViSE promotes.”
More than 200,000 people worldwide have cochlear implants and the number of newly implanted recipients is increasing dramatically each year. All recipients from the newly implanted to the long-term user could experience better hearing with Vanderbilt’s new programming process.
Although cochlear implants are considered standard-of-care treatment for severe-to-profound hearing loss, the quality of hearing is not on par with normal fidelity and a number of recipients may experience only marginal hearing restoration.
Vanderbilt’s interdisciplinary research team sought to improve those results by drawing on the work of students, professors, and medical professionals from the Vanderbilt University School of Engineering, School of Medicine, Vanderbilt University Medical Center, and Vanderbilt Bill Wilkerson Center. In addition to Dawant, the team included René H. Gifford, audiologist and assistant professor of hearing and speech sciences; Robert F. Labadie, associate professor of otolaryngology and associate professor of biomedical engineering; and PhD. student Jack H. Noble, now graduated and a research assistant professor in electrical engineering and computer science.
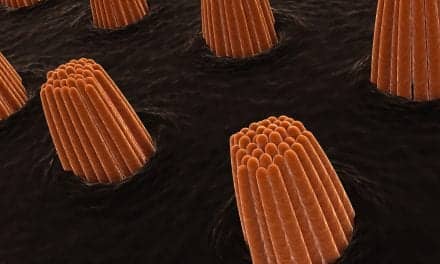
Cochlear implants use 12 to 22 electrodes, depending on the device manufacturer. Although the implanted electrodes can be seen on a CT scan, the nerve cells they stimulate are not easily identified due to their locations and microscopic size (on the order of one millionth of a meter). Traditionally, all the electrodes are turned on and programmed to stimulate any surrounding nerve cells. This one-size-fits-all approach can result in less-than-clear hearing when adjacent electrodes stimulate the same region of nerve cells. Complicating the challenge is that each person’s anatomical structure varies and thus every implant must be programmed — commonly termed as “mapped” — in a comprehensive, time-consuming process postoperatively.
Vanderbilt’s research project included several stages. One was to determine a reliable method of locating spiral ganglion nerve cells (which connect to the auditory nerve) by mapping the corresponding external cochlear anatomy using a statistical shape model and to determine the position of the electrodes with respect to these nerve cells. Achieving this, the next step was to develop a technique that would use the information to generate a customized plan for postoperative cochlear implant programming that could be implemented by individual audiologists in almost any patient.

|
|
From left: René H. Gifford, audiologist and assistant professor of hearing and speech sciences, adjusts the external sound processor worn by patient and study subject Ally Sisler-Dinwiddie. Sisler-Dinwiddie says that having her cochlear implant remapped using Vanderbilt’s new process has made a huge difference in her quality of life. (John Russell / Vanderbilt) |
The new automatic technique uses patients’ pre- and post-operative CT scans to determine the location of the implanted electrodes and where overlap is occurring, possibly causing interference in the transmission of signals. The image-guided strategy and software, which Noble developed as a PhD student, then pinpoint which electrodes can be turned off without loss of hearing fidelity — and in fact, improving it. An audiologist uses this programming plan to create a revised custom map for that person’s needs. The process is completely noninvasive — no surgery is required — and can be accomplished in one office appointment.
The new programming seeks to improve sound quality and spectral resolution (frequency selectivity). “Spectral resolution is basically your ability to take a complex sound and break it down into its individual components,” Gifford said. “It’s something we do very well with the normal-hearing ear and it’s something that the electric-hearing ear with an implant does poorly.”
“If you can improve one’s spectral resolution, what that typically translates to is better speech recognition in noise,” Gifford said. “That’s the holy grail of research. There have been no consistently significant improvements in spectral resolution for implant patients since the introduction of CIS [a speech-coding strategy] in 1991.”
Participant Kelly Harris said the reprogramming improved her hearing so much, it was almost as great as getting the implant in the first place. “I love it. When I left the clinic the day René changed the program, I immediately knew I could hear better,” Harris said. “Before the reprogram, I never knew which direction sound came from. Just last night, my friend thought my TV was making a noise and I knew that it was coming from the other direction. I am also hearing lots more soft sounds and even more music.”
Ally Sisler-Dinwiddie, herself an audiologist, has had cochlear implants in both ears since 2006. The study focused on adjusting her right implant, which provided poor results before the study. “The overall sound quality of my right ear used to be somewhat monotone — anytime someone talked, it sounded like they had a mouth full of marshmallows,” Sisler-Dinwiddie said. “While the overall volume of my right ear was always balanced with my left ear, it lacked the crispness and clarity that my left ear was always right on target with.” She said it’s like the difference between night and day since she participated in the study. “I can tell speech is clearer and a lot more crisp. I can now pick out the intonation in one’s voice with my right ear alone,” she said. “My confidence has soared since the moment I realized I’m actually able to understand speech in a noisy restaurant without relying on my left ear anymore.”
The project continues to enroll new study participants. Currently, they are recruiting adults, although Gifford, who is also director of pediatric audiology and audiology director of the cochlear implant program at Vanderbilt, said that she believes children in particular will benefit from the new programming because it can be mapped with or without responses from the patient.
Cochlear implant recipients can find additional information at vanderbilt.edu/CAOS/research-projects/.
Harris said she has encouraged several people to try the reprogramming. “They should know that it only takes a short time to do this reprogram, and if they are not hearing well with their current processor, they should give it a try,” Harris said. “A lot of people don’t want their programs messed with. I really understand this feeling — usually I am very cautious about changes, but this one worked out to my advantage.”
Gifford said that if patients try the new mapping and don’t like the results, they can have their old programs put back on the implant.
SOURCE: Vanderbilt University