Business Management | January 2018 Hearing Review
While there are managed care programs that make sense for your patients and your practice, the author advocates for carefully analyzing each program and making an informed decision before agreeing to participate, rather than simply enrolling out of a sense of fear.
The concept of over-the-counter (OTC) hearing aids is extremely controversial within the audiology community. I know better than anyone, as I have been figuratively beaten up for my stance on these devices. Many believe that these devices and their accompanying delivery model will have a detrimental effect on the profession and its financial viability. Detractors believe that hearing aid consumers will seek self-evaluation, self-fitting, and self-management, and will not seek evaluation or treatment from professionals.
But, is all provider-directed care beneficial to the consumer and the provider? The hearing aid market is not only being flooded with OTC and direct-to-consumer (DTC) hearing aids, personal sound amplification products (PSAPs), and hearables, it is also being flooded by third-party administrators (TPAs) or hearing aid referral networks who market and offer provider-driven care. I noted at least 14 of these programs are currently operating in the United States.
Third-party administrators are middle-men between the provider and the insurer, employer, or membership group who negotiate discounts, coverage, and benefits for the group and administer the discount or benefit offerings. Hearing aid referral networks are typically online entities who market, via the Internet and social media, significantly reduced, inclusive discount pricing to consumers, have the consumers purchase these devices directly from them, and then refer those consumers to registered, in-network providers for fitting and service. Some of these referral entities do not even seem to require an evaluation—which is funny given the same manufacturer’s aversion to OTC devices and alleged support of provider-driven care.
What the third-party administrators and hearing aid referral networks have in common is this: they insinuate themselves within the delivery model, sometimes undercutting a provider’s previously existing arrangements, and then dictate both care and reimbursement. They do this and then ask providers to join and provide the care to the consumer that they cannot. The saddest fact, however, is that audiologists and hearing aid specialists are joining these programs in droves.
So, why are audiologists (and other providers) willing to join programs that often do not require or allow reimbursement for evaluations and that dictate the care they can provide and what they can collect or receive for the provision of that care, sometimes indefinitely? And why then are many of these same audiologists opposed to OTC devices, which may or may not require an evaluation from a provider, but which ultimately allow the provider to continue to dictate the level and type of care they provide and the fees they determine to be necessary to break even and make a profit? This latter question baffles me.
I make this point because these entities have just as great, if not greater, impact on our profession and our practices than I believe will occur from OTC devices. Right now in this country, without any change to the Food and Drug Administration (FDA) regulatory guidance on what constitutes a hearing aid, literally every consumer has access to discounted amplification. All they have to do is look online for a program. All of these discounts are provided on the work of audiologists and hearing aid specialists.
Our Own Worst Enemy
It should also be pointed out that, as someone who used to work for one of these entities, the shear existence of these programs is partially our fault. We vehemently refused to itemize or offer any form of price transparency. We failed to offer value-based or affordable solutions to consumers. We provided free evaluations and failed to routinely adhere to evidence-based care. And, finally, there were some of us who ignored our managed care agreements and played a dangerous insurance game where every hearing aid patient was pressured to pay for an upgrade; where we billed for hearing aids we had not fit and would not fit until payment was received; where we had the patient pay in full, upfront, even though they had a benefit; or where we charged the payer differently than we charged our general patient population. Insurers, employers, worker’s compensation plans, and, most importantly, consumers, got tired of the game and got tired of losing. Ultimately, they pushed for a lower-cost defined delivery system. Now, the main losers in the current game are the hearing healthcare providers themselves.
So…What Do We Do?
To be clear, I am not saying all of these TPA entities are evil and that providers should not enroll in them. Some actually can and do offer a win-win-win proposition for the consumer, provider, and TPA—especially compared to the system and reimbursement many providers are faced with when dealing with the insurer directly through their own managed care agreements. Some also offer the hearing healthcare provider access to a managed care network in which they might not otherwise be able to participate.
However, unfortunately, that is not what leads most of us to join. A large percentage of hearing care providers just react when a program becomes available or enters their market—they sign up randomly without ever fully evaluating the programs and its cost-versus-benefit to both the provider and the patient. Rest assured that there are programs out there now where the only winner is the middleman. These programs will not go away; they will continue to exist, thrive, and multiply as long as there are providers and consumers willing to accept their products, terms, and payments. When we participate in programs that are not good for both our practices and our patients then we become, yet again, our own worst enemy.
I want this article to be a wake-up call to all hearing care professionals to truly evaluate each program before agreeing to participate. Alternatively, if you are already enrolled, evaluate the merits and the pros and cons of participation, or lack thereof.
There are ways to compete against these entities. There are also ways to legitimately thrive in managed care. I teach audiologists to do this all the time. It just takes education, processes, and a change in mindset.
Success moving forward will also require providers to evolve and accept some inevitable truths:
- Providers will have to itemize, as most of these entities require itemized care;
- Providers will have to be able to justify to the patient the value and costs of the care provided, and
- Providers will have to accept less than their upfront, full-fee, bundled, usual, and customary rates.
However, on the other hand, providers will receive compensation for their services at their rates for the items or services they actually provided. Providers may just not be prepaid for care they may or may not actually render.
I say two things all the time. One is a quote from Dr Phil: “You cannot change what you do not acknowledge.” Audiologists (and hearing aid specialists) have got to stop the pity party, and instead start being proactive in taking steps to respond to our changing competitive landscape.
The second is my own quote: “I could care less what each audiologist or hearing care provider decides to do in the end. All I care about is that they make an informed decision and not one based upon fear.” Educate yourselves. Read the proceedings of what is happening in the industry and the latest research. Truly listen to what consumers are saying. Do not react based upon fear but, rather, fact. I promise providers that, if they do those things, their chance of long-term success multiplies tenfold.
Biography: Kim Cavitt, AuD, was a clinical audiologist and preceptor at The Ohio State University and Northwestern University for the first 10 years of her career. Since 2001, she has operated her own audiology consulting firm, Audiology Resources Inc in Chicago, which provides comprehensive operational, compliance, and reimbursement consulting services to hearing healthcare providers. She is a Past President of the Academy of Doctors of Audiology (ADA) and currently serves as the Interim Chair of the Audiology Quality Consortium (AQC), Vice-President of Government Affairs for the Illinois Academy of Audiology, and is the Chair of the State of Illinois Speech Pathology and Audiology Licensure Board. She also serves on committees through ADA, AAA, and ASHA, and is an Adjunct Lecturer and Clinical Placement Coordinator at Northwestern University.
Correspondence can be addressed to can be addressed to Dr Cavitt, at: [email protected]
Original citation for this article: Cavitt K. Managed care: Some caveats and common sense for hearing care professionals. Hearing Review. 2018;25(1):28-29.
ALSO SEE…In the same issue, Austin Singleton and Patty Greene of TruHearing’s article, Managed Care: Threat or Opportunity.





It was nice to find out what the problem is with my insurance provider- thanks
I’m going through Tru Hearing to use my UAW retiree benefits. They told me who to go to. I waited a 1/2 hour for my hearing test, then another half hour for my fitting- I was out the door in about 40 minutes- he made one adjustment to lower the gain in my left hearing aid to equalize the volume. Over the next week, I tried them, but they were very uncomfortable with his office settings, so I used the Iphone to turn them down by a -2 to -4.
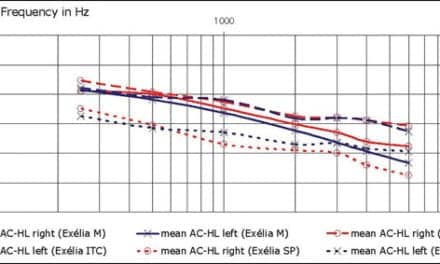
I was talked into getting the highest level Oticon hearing aid as my copay was only $1350 vs a normal price of $6800. My SRT was 40% and 25%. I have mild to severe hearing loss from auto plant industrial noise- sloping to severe at 3500hz and higher.
The flagship hearing aids were just overkill for me, – anyway when I returned for my check, I again was told the Dr was running late- Hmm, I saw his next appt was sitting next to me- I just blurted out to the receptionist, ” I’m just here to turn these hearing aids in”-
I have since learned that I should not have been wearing them all day long to start- no wonder my brain was exploding.
I called Tru Hearing and got a new provider appt.- in my town, not a 1/2 hour drive. I told them I don’t care how long I have to wait for this new appt. -I was 3 weeks out.- they scheduled me for 4pm on valentines day– haha- a slow afternoon, i guess.
Meanwhile, I have really educated myself over the past two weeks.I even know why I might need a recruitment test.
I think my first hearing test was inaccurate- – as I could hear some construction across the street in his testing room, plus I think my tinnitus was interfering with the test- the next time I will ask for double beeps ( I found out that can help and hopefully, this location will be quieter.)
I have researched the technical aspects of all the free options available to me and I will choose the Starkey Livio 1200 rechargeable. I lead a very quiet lifestyle and have decided the premium ones are just overkill for me.
This is your competition– https://www.nuheara.com/usa/products/iqbuds-max/
I ordered them to try out, I think they may be better for some activities-
OMG! I could not have said it better! This is a must read for all hearing healthcare providers, audiologists and dispensers alike. Assess what you are being paid by these companies and determine whether or not it’s worth your time. Analyze your cost of operations (billable hour), and if the reimbursement rate is less than you billable hour, realize that you’re LOSING money every time you see these patients, not being paid what you’re worth.
As Dr. Cavitt stated, we put ourselves in this position and we are our own worst enemies. Quit crying about it and start doing something about it. If you a begrudging provider for these companies and hate it every time you see one of their patient’s in your schedule, then you really need to evaluate why. It’s not the patient that the problem, it’s the system that we unwittingly helped create by not charging appropriately for our services. We placed all value on the products rather than our own skills, and now that’s being used against us. Don’t like it? Do something about it!