Hearing Aid Fitting | March 2020 Hearing Review
By Donald Hayes, PhD
When Joe Sweet decided to pursue curling to improve his cardiovascular health, he did not expect to find out that he also suffered from hearing loss. He was unable to hear what the skip was saying, making it difficult to excel in the sport and socialize with his colleagues. The gradual hearing loss Joe experienced was compounded by the fact that every time he tried a hearing aid, it was either uncomfortable, too loud, or itchy. These hearing devices all ended up in Joe’s bedside table, while outside he continued to suffer in silence.
Joe isn’t alone. Approximately one-third of people in North America between the ages of 65 and 75—and one-half of those age 75 and older—suffer from some degree of hearing loss.1 Perhaps even more alarming is the fact that 80% of those suffering from hearing loss are not wearing the proper aids and devices that could provide drastic improvements to their hearing experience.2
In the midst of an industry-wide transformation, a new first-fit strategy is needed to see higher adoption numbers of this critical adaptive technology.
Obstacles in Hearing Aid Acceptance
Hearing aids are evolving from medical devices to wearable consumer electronics, with technology advancing to include Bluetooth connectivity, TV and music streaming, and secure data logging. These new offerings have expanded the prospective client base and made the hearing aid shopping experience more rewarding for those struggling to cope with hearing loss.
But hearing care professionals still face obstacles when it comes to fitting patients with these devices. While the primary goal of a hearing aid is to optimize a patient’s hearing, the historic fitting process fails to take into consideration the innate tension between wanting to give a person the best speech intelligibility and the reality of what they are ready to hear.
Traditionally, when a patient is fitted for a hearing aid, the healthcare professional aims to create the most optimal fit. This maximizes speech intelligibility, providing enough amplification to hear both high- and low-frequency sounds right out of the box.
The problem they face is that hearing loss has a gradual onset occurring over many years. The longer a person has significant hearing loss, the more they have adapted to a diminished auditory world. It is hard for them to accept the sudden application of appropriate amplification because it is so much louder than how they remember everything being. When you are dealing with a patient who has never worn a hearing aid but suffers from hearing loss, the sudden jolt to their auditory system is alarming and can deter them from wearing a hearing aid in the future. This is how the devices end up on the nightstand.
Consequences of “Failed Fittings”
The consequences of an improper fitting experience can be devastating. Those experiencing a loss of hearing may be forever deterred from properly addressing the issue. Poor hearing health can impact an individual’s physical well-being as well as their socio-economic level. A recent study conducted by researchers at Johns Hopkins found that untreated hearing loss increases the risk of dementia by up to 50% compared to those without hearing loss.3 The study also found greater incidents of slips and falls, high blood pressure, and cardiovascular disease. Depression rates also increased by 40% in five years for adults suffering from hearing loss.
Hearing impairment also triggers structural changes in the brain. The average person loses their hearing over time, but there is enough redundancy within the brain to fill in the blanks when that person can no longer understand every word in a sentence. When a little hearing sensitivity is lost, we work just a bit harder to piece together what we do hear and fill in the blanks based on the context of the discussion. Each time our hearing sensitivity drops a little more, we will again work just a little harder to piece it together, but with slightly less information. Eventually, hearing loss reaches a point where the brain can no longer fill in the blanks, forcing people to exert a great deal of their energy and brain power on listening and impacting their well-being.
Unaddressed hearing loss can also pose significant socio-economic concerns. According to a study by the Better Hearing Institute, adults with hearing loss are more likely to be unemployed and, on average, earn approximately $12,000 less annually than those without significant hearing loss.4 The estimated cost of lost earnings to the US economy is $122 billion, which results in an estimated $18 billion of unrealized federal taxes.
Rethinking the “First Fit” Approach
Audiologists and hearing aid specialists need to rethink the “first fit” approach to hearing aids. Adapting the “first fit” experience to be more reflective of a patient’s gradual hearing loss experience is an alternative that hearing care professionals should consider when fitting patients for new hearing devices. Pursuing a gradual transition allows the auditory system to receive, process, and accept sounds that have been missing for an amount of time.
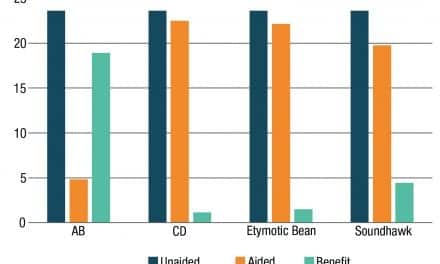
The starting point begins with comfortable natural sound and enough amplification to provide benefit that is not jarring or overly loud. Over the next few days, as the wearer adjusts to the amplification, the devices slowly adjust upwards to the appropriate level that maximizes speech clarity. This gradual transition encourages the wearer to use the devices regularly without rejection due to over-amplification.
Factors that must be considered in this revamped “first fit” approach include calculating the average hearing loss in each ear, a person’s age, and the amount of experience with amplification to determine how much overall gain a patient should receive. Over the span of approximately one month, the hearing device should adapt to the patient’s changing auditory needs, eventually reflecting an industry standard fitting target for the greatest long-term benefit.
The industry is slowly moving towards this “first fit” approach, with companies like Unitron prioritizing a more gradual shift in hearing device capabilities using its Discover platform. But with the senior population in North America expected to double by 2036, it is paramount for healthcare providers to embrace new technologies that will improve hearing health and reduce the associated physical and socio-economic impacts.
References
1. National Institute on Deafness and other Communication Disorders (NIDCD). Age-related hearing loss. September 7, 2018. Available at: https://www.nidcd.nih.gov/health/age-related-hearing-loss
2. Mccormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol. 2013;52(5):360–368. doi: 10.3109/14992027.2013.769066
3. Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011;68(2):214-220. doi:10.1001/archneurol.2010.362
4. Kochkin S. MarkeTrak VII: The Impact of untreated hearing loss on household income. Hear Jour. 2007;60(4):24-51. doi: 10.1097/01.hj.0000285745.08599.7f
Correspondence can be addressed to Dr Hayes at: [email protected]

Image: © Ratpack2 | Dreamstime.com