Recent articles in HR have demonstrated the hearing industry’s ongoing quest for high-quality products and services, emphasizing a need for incorporating evidence-based protocols (or as close as our field can come to this) in the testing and fitting of hearing aids. For example, our June issue featured a MarkeTrak report suggesting that, if every practice in the United States would routinely perform verification (eg, real-ear measurement) and validation (eg, COSI), a total of 521,779 repeat visits for hearing aid readjustments could be eliminated. I pointed out in last month’s editorial that, if you consider that a dispensing professional accounts for an average of $144 per hour in gross revenues (according to Part 1 of the Phonak Marketing Survey), that represents about $56.3 million in revenues for dispensing offices nationwide. So, although patient care issues are always the foremost reason for improving service, it’s clear that V & V and evidence-based protocols can also greatly influence the bottom line and financial viability of a dispensing practice, as well.
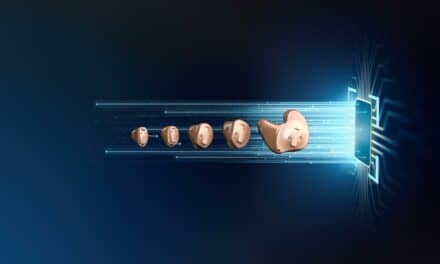
The article this month by audiologist Brian Taylor, AuD, of Unitron and Hearing Industries Association (HIA) Executive Director Carole Rogin makes the important point that employing a best-practices protocol is also a matter of differentiating your market and ensuring that your practice is safeguarded from future competitors—both traditional and nontraditional. Whether we like it or not, personal sound amplification products (PSAPs) and over-the-counter and mail-order/online hearing aids will continue to grow in popularity via the Internet, mass retail stores, and new mediums like mobile device apps. In my November 2009 and June 2010 editorials, I railed about how it’s essentially unfair, from a regulatory standpoint, that these devices can be mass-marketed (with a wink and a nod) to people with hearing impairment, while our industry is required to jump through hoops and spend millions of dollars to bring its products to hearing-impaired consumers.
Although it’s true that PSAPs and similar devices cannot provide anywhere near the same level of performance as professionally prescribed and custom-fit hearing aids, most of them do provide basic amplification—at a rock-bottom price that would bankrupt most professional practices. MarkeTrak VIII estimates that there are some 1.2 million users of PSAPs (see June 2010 HR) versus approximately 8.4 million hearing aid users. So, ultimately, if the FDA isn’t going to regulate PSAPs that increasingly resemble (and are deftly marketed to mimic) professionally fit hearing aids, then our field needs to make sure we continue to differentiate our products and services from these ersatz hearing aids. And, as Taylor and Rogin point out, the #1 way to do this is for the “hearing care professional to deliver personalized care using protocols supported by good clinical evidence [which] has been shown to improve satisfaction and loyalty. Professionals with both the skill and will to differentiate their practice on quality will continue to enjoy a significant competitive advantage as well as the ability to command a premium price for their products and services.” Harvey Abrams, PhD, and colleagues summed up this idea in a June 2007 HR article, appropriately titled “The Future of Hearing Health Care Delivery“:
The successful hearing care practices of the future will be those that have moved from product-based to service-based, with the service focusing on all aspects of the patient’s hearing loss and treatment, including rehabilitation. To this end, the more that patients can understand that hearing instruments in and of themselves do not provide a complete solution to their hearing difficulties, the more they will value the additional services not found through nontraditional hearing instrument channels, such as the Internet and consumer electronics stores.
In my opinion, the future of professional hearing care is extremely bright: a burgeoning aging population and incredible hearing testing, fitting, and device technology. But, if you look at Figure 1 of Taylor and Rogin from our cover story and then keep in mind that disruptive technologies will continue to emerge and compete with the lowest 1 to 3 deciles, it’s apparent that quality service and patient care will be the keys to value and differentiation in hearing health care.
Karl Strom
Editor-In-Chief