Cochlear implants can lead to life-altering improvements in hearing and quality of life. If an older adult candidate questions, “I’m too old for a cochlear implant. What if I only live one more year?” our response is, “What do you wish to do with this last year of your life?”
Cochlear Implants | August 2017 Hearing Review
Advanced age is not a contraindication for CIs. But some things should be kept in mind…
The number of older adults who are pursuing cochlear implantation is rising steadily and represents a growing percentage of total cochlear implants. However, the management of cochlear implant candidates in their 80s and 90s evolves as they advance in age. This population has distinct medical considerations and may experience physical and cognitive changes that may impact their ability to use and troubleshoot the external audio processor. Treatment is further complicated if patients are lost to follow-up due to driving restrictions or changes in caregiver support.
Advanced age is not a contraindication to cochlear implantation. Research has shown that geriatric cochlear implant recipients experience an improvement in speech perception and quality of life postoperatively, including psychosocial benefits such as renewed confidence to participate in social activities and greater independence.
What are age-specific concerns related to cochlear implantation and how can they be addressed? Clinicians and researchers in the Department of Otolarygnology/Head and Neck Surgery at the University of North Carolina at Chapel Hill and in the Department of Audiology at UNC HealthCare conducted a retrospective review of cochlear implant recipients over 80 years of age to assess management considerations in geriatric patients and determine how to improve the care of older adult cochlear implant recipients.
Medical Concerns Related to Age
Older adult cochlear implant candidates have additional medical considerations as compared to younger adults. Older adults require special attention to anesthesia and may require a longer stay in the hospital, as opposed to younger recipients undergoing this type of outpatient surgery. In general, the older the patient, the more likely they are to have had other surgeries and live with comorbid, chronic health conditions. Therefore, it’s especially important to coordinate with specialists outside of otolaryngology to provide a complete picture of the patient’s health.
Specific considerations prior to surgery include blood work, arranging for hospital admission and overnight stay, anesthesia and pain control protocols for geriatric patients, urinary function, and evaluation of overall cognitive status. Postoperative issues noted in this patient population included breakdown of the skin between coil and receiver and damage to external equipment due to falls, indicating potential mobility and balance issues that should be evaluated.
Dexterity Issues, Vision Loss, and Cognitive Decline
Dexterity issues can affect handling of the audio processor and tasks like manipulating program/volume buttons and changing batteries. One way to address this is having access to a remote like MED-EL’s FineTuner, which has large buttons and allows recipients to make changes to settings at their convenience. Raised buttons on the remote control can also help to address vision loss. Further, clinicians address potential dexterity issues by questioning whether the patient is left- or right-handed during the initial cochlear implant evaluation. If both ears meet candidacy criteria, clinicians consider which hand has greater comfort and ease for placing the processor on the side that is more comfortable.
Audiologists can modify the programming of the audio processor and the activation of specific device features to limit confusion and set the stage for greater success in this patient population. The audiologist may select to vary programs only by comfort levels and/or volume settings as the patient acclimates to the sound quality within the first months of listening experience. Once speech perception has stabilized, the number of available programs may be limited to the one or two maps that provide the patient with the best speech perception. The audiologist may also decide to deactivate features, such as sensitivity, so that the listener does not reduce this setting to a range that could negatively influence his or her speech perception with the device.
The processor and remote control will be new technology for the recipient, and the learning curve may be longer for older adults. To increase the level of comfort with the device, clinicians offer additional training in small groups to review features, answer questions, and troubleshoot. The UNC Cochlear Implant Team also developed a simple contact sheet with the most important details at a glance, including clinic and manufacturers’ contacts and phone numbers; this practical and easy tool can go a long way in helping to increase older adults’ comfort level and helping them feel supported.
Cochlear implant teams may need to modify the follow-up schedule for older adults considering potential cognitive issues. A modified follow-up schedule and offering appointments for one-on-one counseling may improve their understanding of how to manipulate the audio processor and remote control. For older adult patients, our program schedules a follow up two weeks after the initial fitting instead of the more routine four weeks. We repeat the counseling that was conducted at first fitting and perform a condensed assessment. Then we schedule follow-up appointments at the 4-week, 3-month, 6-month, and 12-month post-activation intervals.
Loss to Follow-up
The UNC Cochlear Implant Team advises all patients to return to the clinic annually for assessment of speech perception abilities, mapping of the audio processor, and medical follow-up, if needed. The review of our older adult cochlear implant recipients found that the most common issue post-surgery was loss to follow-up, which accounted for nearly a quarter of those 80 years of age and older. Transportation challenges were a key contributor. There is also the potential for limited ability or inability to follow-up, particularly if the recipient is in a long-term care facility.
The importance of attending follow-up appointments should be discussed during the evaluation period. Follow-up assessment and programming is an important part of the process and is a factor in the recipients’ overall success. Attending routine follow-up appointments may also prevent confusion regarding manipulation of the device, and breakdown of the skin between the coil and receiver. Having an open dialogue is critical regarding who will be there for transportation and support at home for the recipients. When candidates first come in they may be at a point where they can drive, but it’s important to ask about driving restrictions currently in place or anticipated. The ability to return for routine follow-up care may be limited when traveling becomes difficult.
Telemedicine for facilitating follow-up. Distance to the cochlear implant center may also influence the potential to follow-up by older adult patients, who may be relying on others for transportation. Options to prevent or optimally manage patients who cannot return to the cochlear implant center due to distance include telemedicine, and partnering with and training staff at satellite locations. The issue of inability to follow-up due to distance would be minimized if cochlear implant teams collaborate with physicians and audiologists at satellite offices. The cochlear implant team would be responsible for conducting the cochlear implantation procedure, initial activation of the audio processor, and making mapping adjustments to achieve stability of speech perception within the initial months of listening experience. Teams at the satellite offices would be responsible for annual follow-up testing and mapping, medical follow-up, and referring to the cochlear implant center if issues present.
By having a local contact closer to home, medical or device problems can be detected earlier and referred to the main cochlear implant center for resolution, and recipients can continue to be followed. This is also clearly a logistical benefit for patients. Over the past several years, UNC has been a part of a national trend where large medical centers and hospitals expand regionally to satellite locations to widen their network.
Conclusion
Older adult recipients can experience significant benefit from cochlear implantation, but often have special medical, physical, and logistical considerations. Modified follow-up schedules, and additional training and materials may help with dexterity, visual, and cognitive issues.
Cases that return to the cochlear implant center for follow-up are treated with appropriate medical management, device assessment, programming, and counseling. The prevalence of cases not returning for follow-up, coupled with new management considerations in this age group, is a concern that physicians and audiologists working with this population should recognize. Medical centers can prevent complications in patients with travel limitations through telemedicine and by training staff at satellite locations to recognize medical considerations of octo- and non-agenarian cochlear implant recipients. Providing routine care locally, while referring to the primary center when warranted, may improve the long-term management of this population.
Cochlear implants can lead to life-altering improvements in hearing and quality of life. If an older adult candidate questions, “I’m too old for a cochlear implant. What if I only live one more year?” our response is, “What do you wish to do with this last year of your life?”
Acknowledgements
Dr King is a consultant on MED-EL’s Audiology Advisory Board, and Dr Pillsbury is a consultant on MED-EL’s Surgical Advisory Board. Drs Dillon and Rooth have supported a research grant for MED-EL.
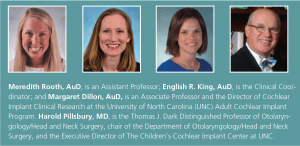
Biography: Meredith Rooth, AuD, is an Assistant Professor; English R. King, AuD, is the Clinical Coordinator; and Margaret Dillon, AuD, is an Associate Professor and the Director of Cochlear Implant Clinical Research at the University of North Carolina (UNC) Adult Cochlear Implant Program. Harold Pillsbury, MD, is the Thomas J. Dark Distinguished Professor of Otolaryngology/Head and Neck Surgery, chair of the Department of Otolaryngology/Head and Neck Surgery, and the Executive Director of The Children’s Cochlear Implant Center at UNC.
Correspondence to Dr Rooth at: [email protected]
Citation for this article: Rooth M, King ER, Dillon M, Pillsbury H. Management considerations for cochlear implant recipients in their 80s and 90s. Hearing Review. 2017;24(8):28-30.