Staff Standpoint | May 2021 Hearing Review
By Karl Strom
We need to celebrate the victories. The recent progress in advocacy about the links between diabetes and hearing loss has been impressive. The US Centers for Disease Control and Prevention (CDC) has just published a terrific 2-page handout, “Take Charge of Your Diabetes: Healthy Ears” that informs people with diabetes about their susceptibility to hearing loss and balance problems. Likewise, the American Diabetes Association (ADA) in December recognized hearing loss as being more common in people with diabetes and added audiology to its table on referrals for initial diabetes care management in its recent updated Standards of Medical Care in Diabetes-2021. Additionally, The Audiology Project (TAP)—which has been largely responsible for these victories—will be involved in a webinar that will be available on the CDC’s website, according to Kathy Dowd, AuD, who with her TAP colleagues have championed this issue (see our feature article).
Informing the public about the links between hearing loss, diabetes, and other comorbidities is important for at least three reasons:
1) Improved healthcare for patients. As Christopher Spankovich, PhD, notes on page 16, patients who understand they are at higher risk for hearing loss due to a chronic disease like diabetes can be extra-diligent in reducing their exposure to other hearing loss risk factors, such as loud noise. Additionally, knowing that hearing loss may be a warning sign for other chronic illnesses could pave the way for earlier intervention and better overall health for your patients.
2) Reducing medical costs. However good or bad it may be, the cost of medical care in the United States is easily one of our largest problems as a nation. The author of the cover article, Lena Kauffman, has written extensively about outcomes-based reimbursement models in medicine and published a Hearing Review special report titled “Hearing and Value-based Healthcare” that shows why better hearing could play a substantial role in reducing healthcare costs.
3) Working more closely with physicians. As Victor Bray, PhD, points out in this issue, hearing care professionals have an important role on the patient’s healthcare team. Becoming a prominent player of that team means better care for the patient and more referrals for the professional.
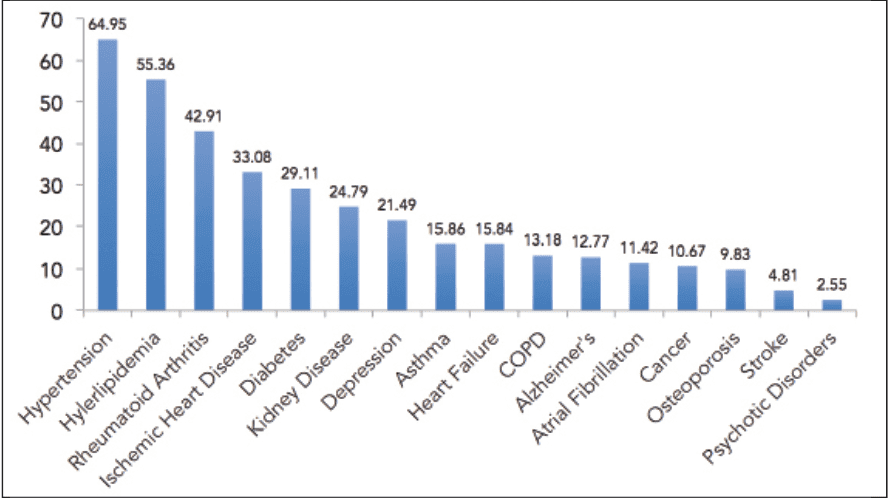
In our March 2021 edition, Ian Windmill, PhD, and Barry Freeman, PhD—two former presidents of the American Academy of Audiology (AAA)—published an article about trends in Medicare audiologic procedures. In Figure 7 of that article (reprinted above), they showed the percentage of audiology patients with various comorbidities. It’s a stunning graph and may serve as a roadmap for future advocacy efforts. More than 1-in-5 patients have cardiovascular-related diseases, diabetes, kidney disease, and/or depression. Given these comorbidities and their links to hearing loss, we may need a TAP-like initiative for each. And more victories.
About the author: Karl Strom is editor of The Hearing Review and has been reporting on hearing healthcare issues for over 25 years.
Citation for this article: Strom K. Comorbidities and hearing care. Hearing Review. 2021;28(5):6.





