In a recent survey of 2,000 UK adults commissioned by the British Irish Hearing Instrument Manufacturers Association (BIHIMA), consumers were questioned about their awareness of the co-existence of hearing loss and other diseases such as dementia, depression, cardiovascular disease, diabetes, and high blood pressure. BIHIMA announced the results in a press release.
In a second survey of audiologists, BIHIMA found that 85% of hearing care professionals did not think their patients were aware of co-existing conditions.
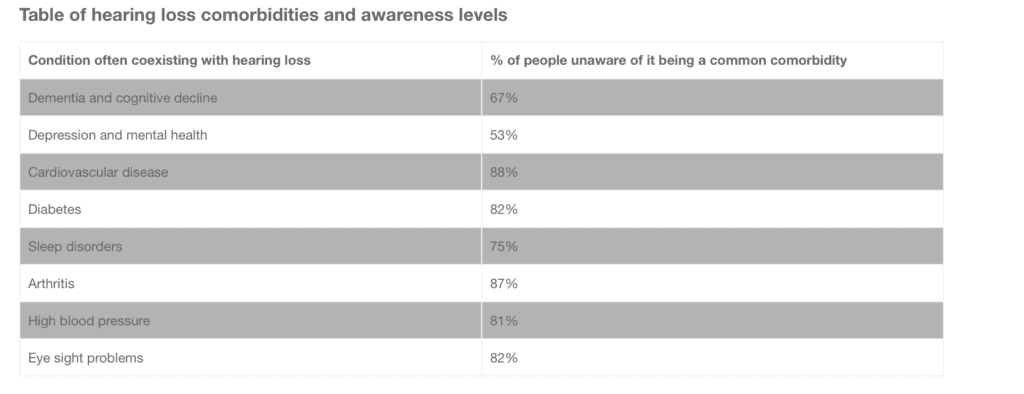
Significantly, the data showed that 67% of people are unaware that untreated hearing loss can contribute to early onset dementia. On top of that, over half (53%) said that they had no idea that hearing loss can cause depression and other mental health problems.
Co-existing Conditions
The research also looked at the link between hearing loss and other co-existing medical issues (although with these conditions it is not necessarily known how or if one causes the other). For example, 88% of respondents were unaware of the association of hearing loss with cardiovascular disease. A further 82% did not know of the link with diabetes, and three quarters (75%) were clueless about the association with sleep disorders.
This lack of understanding also extended to other comorbidities (see table below).
Interestingly, the data also showed that the age group with the least awareness were those aged between 45-54 (only 19% knew that hearing loss is a comorbidity with other health problems), while the younger generation of 16-24 year olds were better informed (47% were aware).
Professional Opinion
This data was confirmed by a survey of audiologists, conducted by BIHIMA, showing that 85% doubted their patients’ knowledge of comorbidities.
However, audiologists were slightly more optimistic about societal levels of awareness about the risk of dementia caused by hearing loss, with 51% saying they thought their patients knew about it.
Interestingly, the majority of audiologists (54%) also said they would be very unlikely to speak to their patients GP about potential comorbidities. And 51% said they were not likely to consult with a patient’s GP, consultant, or pharmacist about potential ototoxicity of medication.
A holistic and integrated approach to a patient’s health, which considers the interplay between all medical issues, is likely to be beneficial for patients. BIHIMA’s support of a new educational toolkit for GPs, developed by the RCGP to improve hearing loss care for patients, will help to bridge this gap.
Knowledge Leads to Action
The above research is important in its potential to encourage behavior change: a further 64% of Brits said they would be more likely to wear a hearing instrument if they knew about the association of hearing loss and other health conditions.
It is a clear demonstration, according to BIHIMA, that if people, especially those most at risk, were more aware of the issues associated with hearing loss they would take the problem more seriously and seek treatment. These results also provide motivation for audiologists to be more informative to their patients about potential comorbidities and for medical practitioners to work in collaboration with audiologists.
“This research reveals a concerning lack of understanding amongst the public. We are calling on others in the hearing care sector and the government to help us get the message out there that looking after your hearing can improve so many areas of health, meaning people live well for longer,” said Paul Surridge, BIHIMA chairman.
Research and Methodology:
The first census was conducted by Censuswide across 2,000 UK adults. It was completed in February 2020, but publication was delayed due to the coronavirus outbreak. The second survey was conducted by BIHIMA and canvassed a group of 70 audiologists across England and Ireland in December 2020.
Source: BIHIMA
Image: BIHIMA