When Max Goldstein, MD, returned to St. Louis from Vienna about the time that World War I was getting underway, he probably didn’t realize that he was laying the foundations for what would eventually become one of the preeminent hearing research centers in the U.S. In Vienna, he had learned a technique for teaching speech to children who were deaf, and beginning in 1914, he started teaching speech to deaf children in the upstairs office of his practice. Due to the demand for his services and the time this consumed, his otology practice started foundering, so he began educating area teachers on the oral method of teaching deaf children. As only one of his many legacies (for example, Goldstein also established the medical journal, Laryngoscope, at age 26), the first School for the Deaf building was established in 1916, another was built in 1928, and the third was completed in January 2000.

For the hearing science field, Goldstein’s vision in establishing Central Institute for the Deaf (CID) in St. Louis has yielded nearly a century of important ideas, research and scientific advancements. It would be easy enough to secure CID’s claim-to-fame in the annals of hearing science with the names and work of people like Goldstein, Hallowell Davis, MD, S. Richard Silverman, PhD, and Ira Hirsh, PhD, all of whom served as directors at CID. But when the work of people like Margaret Skinner, PhD, David Pascoe, PhD, James Miller, PhD, William Clark, PhD, Ann Geers, PhD, and many others at CID and nearby Washington University is added, it’s easy to see why the St. Louis area has become known as one of the premiere centers for hearing health care, education and research in the world.
Research Diversity & Synergy
The infrastructure of CID has been enhanced in the past five years with new facilities, scientists and clinicians, as well as an added focus on molecular and neurological research into hearing loss. The new school building and Harold W. Siebens Hearing Research Center are connected, via architectural features and walkway, to the historic school building.
Donald Nielsen, PhD, executive director of CID, attributes much of the success of the Institute to the synergies both within the organization and between CID and Washington University, with whom they have a close working relationship. The Institute serves as the faculty for the university’s Department of Speech and Hearing, and the two campuses are a short walk from each other. He believes that, in particular, the interaction between the medical school faculty, students and CID staff is a factor in making CID unique. “The fact is that our vision isn’t just for CID; our vision is to make St. Louis the center for hearing and deafness in this country,” says Nielsen. “The same type of synergy that we have on the two campuses is what we want throughout the metropolitan area…We have a powerful group of people. As we recruited our biologists, they interviewed with the basic science and ENT departments at the medical school. As a result, all of these people now have joint appointments in the medical school. This, in turn, allows us to recruit students from the university. For example, the neuroscience department—which is one of the best in the country—allows us to have some of the best graduate students in neuroscience working in our laboratories.”
There has also been a deliberate attempt to create an atmosphere that is conducive to scientific exploration, education and collaboration, according to Nielsen. “Our biology group meets two Fridays each month with other groups at the medical center for pizza and discussions on research. These types of interactions have also allowed us to apply for grants together.” Recently, the Institute has benefitted from a large increase in research funding from the National Institutes of Health (NIH), National Institute of Deafness and Communication Disorders (NIDCD), the National Aerospace Agency (NASA) and from several private grants and donations.
|
Facts on CID CID scientists have conducted two landmark NIH studies on cochlear implants in children; researchers in cellular and molecular biology of the ear have recently been awarded 13 competitive grants: 9 from NIH and 4 from NASA. n Educational assessment tools developed by CID for deaf children are used in all 50 states, all Canadian provinces, six Australian provinces and 33 countries worldwide. n CID teaches deaf children from birth through about age 14 to talk, listen and achieve literacy. The U.S. Department of Education has honored the program twice for excellence. One of the CID school’s graduates is Heather Whitestone, the young woman with profound hearing loss who was named Miss America in 1995. CID has nine day and residential programs, and students have come from 48 states and 23 countries. n CID’s clinicians, scientists and teachers of the deaf compose the faculty of the Washington Univ. Department of Speech and Hearing, which is based at CID through a financially independent arrangement. CID has awarded more than 1600 graduate degrees in deaf education, audiology, and speech and hearing sciences. CID graduate students have come from 38 countries and 44 states. They compose one-third of the leaders of OPTION oral schools across North America. During its last ranking of audiology programs in 2000, U.S. News & World Report rated the CID graduate program in the nation’s Top 10. |
Research at CID
Like the House Ear Institute in Los Angeles (see the March 2001 issue of HR), for which Nielsen was executive vice-president of research in the early 90s, CID has added the areas of cochlear hair cell repair, rescue and regeneration research to its long history of applied clinical research. “We made the conscious decision to get started in cellular and molecular biology, with a particular focus on hair cell regeneration,” says Nielsen. “We were already involved in research on cochlear implants in children and adults and how well these devices worked. But we are seeking to leap-frog and get to where the next prosthetic device is going to be. So we’re also focusing on what we think will eventually be a biological prosthesis, and this leads us into the areas of cellular and molecular biology.”
The Siebens Hearing Research Center, directed by Nancy Tye Murray, PhD, includes two research centers, one dealing with biological research and the other focusing on clinically applied research. The Fay and Carl Simons Center for Biology of Hearing and Deafness, which is directed by Richard Baird, PhD, is devoted to research on the repair, rescue and regeneration of inner hair cells. Recent research topics have included developmental mechanisms in the brainstem and inner ear, sensory cell regeneration, the role of free radicals in presbycusis and noise-induced hearing loss, and sensory cell atrophy. Research at the Center for Childhood Deafness and Adult Aural Rehabilitation concentrates on the relationship between hearing and language acquisition, the effectiveness of hearing instruments and cochlear implants, the development of new diagnostic and assessment techniques, aural rehabilitation programs, and issues relating to clinical audiology, psychology and speech-language pathology.
The Institute also has a strong hearing care clinic under the direction of Brad Stach, PhD, who has recently expanded CID’s services to include a network of satellite clinics in St. Louis.
The following is an update on a few of the research projects being undertaken at CID, and is intended only as a sampling of the Institute’s activities. Many more projects and distinguished researchers are involved in important work at CID that could not be covered here due to space restrictions.
Clinically Applied Research
The goal of the Center for Childhood Deafness and Adult Aural Rehabilitation is to focus on applied research with emphasis on the two ends of the life-span continuum: infants and older adults. Four principle researchers are addressing questions that involve language processing and speech development, the creation of audio or visual aids to assist in aural rehab and speechreading training, as well as the development of new audiological diagnostic tools.
Optimal ages for implantation: A five-year NIDCD-funded study headed by Johanna Nicholas, PhD, and colleagues is looking at the language development of children who receive cochlear implants at different ages. Specifically, Nicholas is interested in how language development progresses in children who receive an implant before age 2 compared to those who receive an implant between ages 2 and 3.
“The point of this study,” says Nicholas, “is that there has been a fair amount of research that shows that children who receive a cochlear implant younger than age 5, as compared to over age 5, do much better in terms of developing spoken language. But now we’re looking at that preschool period and asking, ‘What is the best age for a preschool child to get a cochlear implant?’ There are several theoretical reasons to suggest that the earlier you get sound into the brain, the better. Many surgeons are pushing for implantation at younger ages, and anecdotes from teachers in preschool classrooms suggest that children who receive implants at 12-18 months seem to have greater advantages over those implanted at older ages.”
The five-year study involves 50 children in the U.S. and Canada who have been implanted at 12-24 months of age or 30-36 months of age, and who are enrolled in either auditory-oral (encouraging speechreading) or auditory-verbal (don’t use speechreading) programs. The research team visits these children when the child is 3.5 years old, and they videotape them and the parents in a play situation that allows for natural language sampling. Using the videotape and parent questionnaires, the researchers obtain a comprehensive analysis of the child’s language and communication abilities. One year later, the researchers return and record the same information when the child is 4.5 years old. At that time, formal language testing is also included in the assessment.
Nicholas says it is important to gain objective data on the efficacy of implantation at different ages, and this study should provide key information for parents faced with the difficult decision of whether and when to have their child undergo surgery to receive a cochlear implant. “It’s obvious that we need more than anecdotes,” says Nicholas. “We need to have a well-controlled study in which everything about the children is well-matched, except the age of implantation…It’s important to understand whether or not it makes a significant difference to get an implant at 12-18 months, for example, versus waiting until 3 years. Understandably, not all parents are ready to jump into a major surgery. We need to be able to tell these parents what the best course of treatment is, and arm them with information based on scientific evidence.”
Value of psychosocial therapy: A grant from Cochlear Corp. brings the Center for Childhood Deafness and Adult Aural Rehabilitation together with the Washington University Medical School in assessing the value of psychosocial therapy for adults who have recently received cochlear implants. The study focuses not only on managing communication difficulties, but also on the positive and negative changes associated with hearing loss and the restoration of some hearing abilities. It looks at groups of 8-10 cochlear implant users and their spouses relative to the potential difficulties that they encounter upon experiencing newfound hearing capabilities. For example, cochlear implant recipients may suddenly become less dependent on their spouse for some daily activities, and this can produce both positive or negative effects.
“Psychosocial therapy is directed toward addressing some of the emotional issues associated with both hearing loss and the successful use of a cochlear implant,” says Tye Murray. “We’re trying to objectively demonstrate the effectiveness of this type of intervention. Our long-term goal is to develop a psychosocial therapy program and manual that can be used throughout the country. Additionally, we plan to expand the scope of this work to not only include implant users, but also hearing aid users. It’s very exciting work. I’ve been in the AR field for about 20 years, and this is one of the [few] truly new ideas I’ve seen in a long time.”
Having objective data on the effectiveness of aural rehabilitation approaches is imperative, according to Tye Murray, who in 1999 published a book entitled Aural Rehabilitation. “I think this has been a traditional failing of aural rehab in many cases,” she says. “We don’t have solid objective data to show its effectiveness, and, consequently, support for it from both hearing facility managers and patients is often lacking.”
Sensory abilities and aging: How aging affects a person’s ability to integrate sensory information is the subject of an NIH-funded study being directed by Nancy Tye Murray. Four groups of young and old people, with and without hearing loss, are being studied to see how hearing loss affects the ability to integrate auditory and visual cues. Preliminary data suggests that aging may not affect the ability to lipread or to visually recognize certain components of speech; however, little data exists on how aging impacts a person’s ability to combine what is seen (viewing of speech gestures) with what is heard. “The real question lies in the amount of integration that is affected by aging more than just the ability to recognize speech visually,” says Tye Murray.
|
Word of Mouth Related to the CID’s research on aural rehabilitation is its Word of Mouth program. Word of Mouth. which originated with Elizabeth Mauze´, PhD, invites older adults to learn communication strategies that will aid them in their active lives. Many of the people participating in the program are executives, board members of institutions and foundations, or hold high-profile appointments. The program provides them with practice in using communication enhancement strategies, common-sense tips in optimizing their listening environments, and practice in lipreading and speechreading. The program now constitutes part of CID’s comprehensive hearing aid orientation program that is overseen by Brad Stach and CID audiologist Kathy Rehwinkel. The Word of Mouth concept has evolved into a four-part CD-ROM program called Conversation Made Easy. Developed by Tye Murray and her colleagues, the CD-ROMs represent one of the first interactive AR tools that can be used for both clinical and take-home instruction. Separate programs exist for adults and children (the children’s version doesn’t require any reading, and neither version requires typing). Program 1 provides basic lipreading training; Program 2 provides practice in synthetic speechreading, or the recognition of sentences through lipreading. The two programs use several different speakers so patients get a more realistic practice listening and interpreting different communication styles. Opportunities exist for participants to ask the talker to re-phrase sentences, elaborate on content, or simplify the message. Programs 3 is situation-specific lipreading in which a number of talkers have been filmed on location. For the adult training session, there are exercises filmed in a shoe store, a restaurant, a party and an office. CID has used the program in-house with clients in the Word of Mouth program and in hearing aid orientation programs, but starting in December the Institute will start making these CD-ROMs available for clinics, schools and individuals with hearing impairment throughout the U.S. “For whatever reason, the fact is that a lot of patients can’t, or won’t, come in to receive oral rehab—many are working during the day and have family obligations in the evenings, or they don’t have transportation,” says Tye Murray. “Our goal is to make these aural rehab programs available in a home setting.” She says that, in the clinic, the program is usually facilitated by a clinician, and it is used with three patients sitting around a computer monitor sharing each other’s ideas for each communication problem. Additionally, the program has proven successful as a take-home AR program for older adults, according to Tye Murray. |
Biological Research
The Fay and Carl Simons Center for Biology and Hearing Deafness includes six scientists researching the molecular and biological aspects of hearing. Since 1998, the Center has gone from a funding level of a few hundred thousand dollars per year to $2 million in 2001, according to Center Director Richard Baird, who has also helped establish the Inner Ear Consortium, a group of 18 scientists from CID, Washington University and St. Louis Univ. The Consortium’s goal is to promote collaboration among inner ear scientists, enhance existing research programs, maintain shared equipment, and support common services for digital imaging, ultrastructural analysis and studies of gene expression.
Baird believes that the overall picture of hair cell research is more complicated than it was 5-10 years ago, but he’s quick to add that this is actually a good thing: “I think a number of different potential recovery processes for hearing loss have been found. We’ve now realized that it may be possible to intervene at different stages, depending on how much damage is caused and when that damage occurs.”
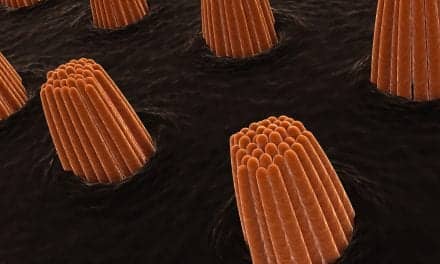
Because of this, many of the researchers at CID are focused on the “3R’s” of hair cell restoration: repair, rescue and regeneration. The repair process, explains Baird, refers to cells that are damaged but can still fix themselves. The rescue process involves those hair cells that have already committed themselves to cell death—a process known as “apoptosis.” Apoptosis is a fairly well understood process in a number of cellular systems, and it now appears that it is possible to block cells from actually carrying it out (i.e., rescuing them from death). Conversely, the regeneration process refers to a situation in which the battle has already been lost: the hair cells are dead or a number of them have disappeared and the challenge is to make new cells. One example of CID research into this avenue includes the work of CID Scientist Mark Warchol, PhD and Gail Neely, PhD, of the Washington University Medical School, who have conducted work on human hair cell regeneration using the two genome centers at the university.
Baird says that hair cell recovery was originally believed to be accomplished by having non-sensory cells re-enter the cell cycle, mitotically dividing and making new cells, some of which become hair cells. More recently, he has shown that hair cell recovery takes place in the bullfrog vestibular organs even when cell proliferation or mitotis is blocked. In other words, the recovery of hair cells is due to a different regenerative mechanism than what has been observed in starlings and other birds.

Although the process was originally believed to be a non-mitotic type of hair cell regeneration, Baird says that he now believes non-mitotic hair cell recovery is due to the self-repair of sublethally damaged hair cells. A similar form of self-repair also is believed to take place in mammalian vestibular organs. Currently, researchers don’t have a good mechanistic explanation for this process, says Baird, but he and his colleagues think it may involve a trauma-induced increase in the level of free oxidative radicals that catalyzes new gene and protein expression in hair cells. The challenge is to understand the biochemical mechanisms underlying lethal and sublethal hair cell damage and the signal transduction cascades of the repair process. Baird will be working with CID Neuroscientist Kevin Ohlemiller, PhD, in research on the regulation of free oxidative radicals in the cochlea to answer these questions.
Presbycusis by cumulative injury: Kevin Ohlemiller is looking at the biochemical and genetic mechanisms behind age-related hearing loss. Much of Ohlemiller’s research is the logical extension of the work done nearly 30 years ago by Harold Schuknecht, a physician who analyzed a large collection of temporal bones from hearing-impaired people. Although he applied several caveats to his work, Schuknecht proposed five general categories of degeneration in temporal bones. These included the degeneration of hair cells (sensory), spiral ganglion (neural), stria vascularis (strial) and various combinations of these categories.
What was intriguing to Ohlemiller was that some of Schuknecht’s categories—particularly the neural and sensory categories—looked to be due to cumulative injury rather than due only to aging. He explains that, if one looks at general theories of aging, two prominent ideas stand out. The first is the free-radical theory of aging which asserts, in simplified terms, that we’re all rusting like a tractor in a field. The other principle of aging is the biological-clock theory, which basically asserts that, over the course of our lives, there is some sort of clock that activates specific genes and deactivates others. This turning on and off of genes somehow contributes to the gradual decay process we know as aging.
Ohlemiller believes that it’s more likely these two theories are simplistic explanations of two opposing ideas. “Usually, when you have two polarized viewpoints, the truth generally lies somewhere in the middle,” he says. “What is probably happening is that the injury processes are driving a genetic program of some kind. A common biochemical mechanism that seems to accompany injury is free-radical production. Some of our work in recent years has focused on demonstrating that cochlear injury due to noise and ototoxins is largely, but not completely, mediated by free radicals.”
Ohlemiller and colleagues from the University of Buffalo looked into the cumulative injury notion of presbycusis by analyzing a strain of mice that were genetically engineered to have defective genes relative to the production of antioxidant enzymes. The study found that these mice were more vulnerable to noise and, as they aged, they showed a kind of cochlear degeneration that resembled Schuknecht’s sensory and neural hearing loss categories.
“It appears that free-radical production has much to do with these types of hearing damage,” says Ohlemiller, “and it’s plausible that the reason some people have certain kinds of presbycusis is that they carry genes that might make them more susceptible to developing some of Schuknecht’s injury categories. Since there are a lot of genes involved in antioxidant protection-type activities, it’s possible that some people who develop sensory presbycusis, as well as others who develop neural presbycusis, do so because they have crippled or reduced antioxidant protection.”
Ohlemiller’s research has also involved Schuknecht’s strial category. A mutation, called Ahl (for Age-related hearing loss), has been found in many strains of mice and has been carefully studied by researchers. In his research, Ohlemiller has shown that BALB mice, which are homozygous for the Ahl mutation, do not develop the strial degeneration that has been observed in similar studies of other mouse strains. “Our research suggests that the results of a Ahl mutation depend on genetic background: if you place Ahl on one strain of mice, the results are different than if you placed it on another strain. So, should this gene be shown to be homologous to humans, it appears that you could have the Ahl mutation and, depending on the rest of your genetic makeup, you may or may not develop hearing loss.”

Hair cell circuitry: What would happen if scientists suddenly discovered a method to repair or create new hair cells? The answer largely depends on whether the afferent (coming from the brain) and efferent (leading to the brain) neurons of those cells are connected properly to the brain. Neuroscientist Dwayne Simmons, PhD, has been conducting research on the development of the synapses of hair cells. He is also looking at how axons connect to sensory hair cells during cellular development, and how efferent neurons make their connections with the organ of Corti.
“What we’ve found has been somewhat surprising,” says Simmons. “Relative to the development of efferent olivocochlear neurons, the dogma in the field basically suggested that the lateral system went to the inner hair cells initially, then the medial system went to the outer hair cells at a later period in development. What our data has suggested is that the medial group actually connects transiently to an interim target, which is the inner hair cell, and then transfers that connection to the outer hair cell at a later time. So, in essence, we’ve been able to propose what we’ve called a “developmental waiting period” that exists within the cochlea, in which brain neurons transiently innervate an interim hair cell target before making connections with the final hair cell target.”
Simmons’ research has also shown that the developmental waiting period occurs in transgenic mice before the end of the first postnatal week. “The system is undergoing an amazing amount of plasticity very early in life, and the question is why?” says Simmons. “Why are these neurons making such a complicated act just to make these connections? Recently, data has emerged that there is a physiological reason for these inner hair cells to be contacted initially by the efferent olivocochlear neurons.”
His research also suggests that this complex wiring act may be necessary for the development of normal hearing. There is evidence that the second efferent system from the brain is undergoing a lot of plasticity at the onset of hearing in the rodent. So, according to Simmons, one system is essentially precocial—it seemingly moves about freely and helps set up the system for proper function, while the second system is timed to undergo a lot of changes at the time of the onset of hearing. “We don’t know if the onset of hearing triggers that second system, or if the second system helps trigger some aspect of the onset of hearing,” he says.
Synapse formation: The above research has led Simmons and Richard Baird to pursue a collaborative project, looking at how synaptic connections are made on repairing and regenerating hair cells. It’s well established that the frog’s auditory system is set up in a highly tonotopic manner, with neurons migrating to specific points during development—all while the animal cannot yet hear.
Cells create new ion channel proteins, and several of the channels have to be placed in close proximity to each other for them to work. The researchers think these ion channels may attract nerve fibers to form synapses at the clusters of ion channels. “It’s not clear if the nerve fibers initiate the contact or whether hair cells somehow draw the nerve fibers to them,” says Baird, who likens the problem to a chicken-or-egg type of question. The team is using a multiphoton confocal microscope and fluorescent dyes to carry out time-lapse studies of ion channel clustering and synapse formation and maturation in living cells.
Simmons says that research on synapse formation is extremely important; until hair cells are connected with nerve fibers, they cannot contribute to hearing in an organism: “At some point in the future of cochlear implants or with a regenerated sensory system, we’ll have to understand how to get the neurons to migrate to very precise locations—or to remain in precise locations if the cells haven’t been destroyed. That requires an understanding of how the neural connections are made in the first place.”

NASA and vestibular systems: On November 29th, the space shuttle Endeavor will be carrying 36 quail eggs that may ultimately help scientists better understand vestibular system development. CID Scientist J. David Dickman, PhD, and Anna Lysakowski, PhD, of the University of Illinois-Chicago have collaborated on a project funded by NASA to examine patterns of vestibular receptor cells and count the otoconia that are involved in balance. They believe that, when subjected to the microgravity of space, the receptors and ear stones of the embryos will become thicker than those of their earthly counterparts because they will be trying to make up for the lack of gravity. Using neural tracer dyes, micro 3D reconstruction and other methods, the team will also observe how developing nerve fibers connect with vestibular receptor cells in microgravity.
It is hoped this data will contribute to the understanding of vestibular disorders such as benign positional vertigo (BPPV) and the bone decalcification and muscle loss experienced by astronauts.
Commitment to Progress
With its biological and clinical research, its clinic and school for the deaf, CID has an epistemological outlook on hearing loss. “I’m extremely proud of everybody here and the work they’ve done,” says Donald Nielsen. “We’ve also had wonderful support from the community. To give you an example, our board members alone have donated over $5 million for our capital campaign and our staff has donated over $140,000. I’ve never worked anywhere in which the staff was that dedicated to their work and organization. It’s a place where everyone is fired up about what they do, they do their jobs well, and they have a lot of respect for each other. All that, combined with the right vision, has taken CID to new heights and we’re still climbing.”
“The magic of CID is its interaction,” says Tye Murray. “In fact, if you come to the cafeteria around noon you’ll see all the people at the center—scientists, lab technicians, clinicians, students, and all the children—in the very same room eating together. We’re always looking for opportunities to cross-pollinate our work between the different areas…With the children present, and having the ability to observe classrooms and talk with the teachers, the scientists understand what the research needs are in the real world…Everyone gets first-hand experience that a lot of people never have. I think there are few facilities that have this intimate bond with what our research objectives are all about: seeing the kids here is motivating and even inspiring.”
“The magic of the place,” says Tye Murray, “is that we do have very good people in their disciplines, but very different disciplines all working side by side. Max Goldstein in the early part of the century had this vision in mind when he founded CID, and I think it still works.”
Acknowledgements
The Hearing Review thanks the CID staff members who took time out of their busy schedules to be interviewed for this article. We also extend special thanks to Nancy Tye Murray, and to Kim Readmond in CID’s Communications Department.
Karl E. Strom is editor of The Hearing Review.