Both high and low frequency hearing impairment have been linked with sleep apnea in a new study of nearly 14,000 individuals presented this week at the 2014 American Thoracic Society International Conference in San Diego.
“In our population-based study of 13,967 subjects from the Hispanic Community Health Study/Study of Latinos, we found that sleep apnea was independently associated with hearing impairment at both high and low frequencies after adjustment for other possible causes of hearing loss,” said lead author Amit Chopra, MD, currently at the Albany Medical Center in New York.

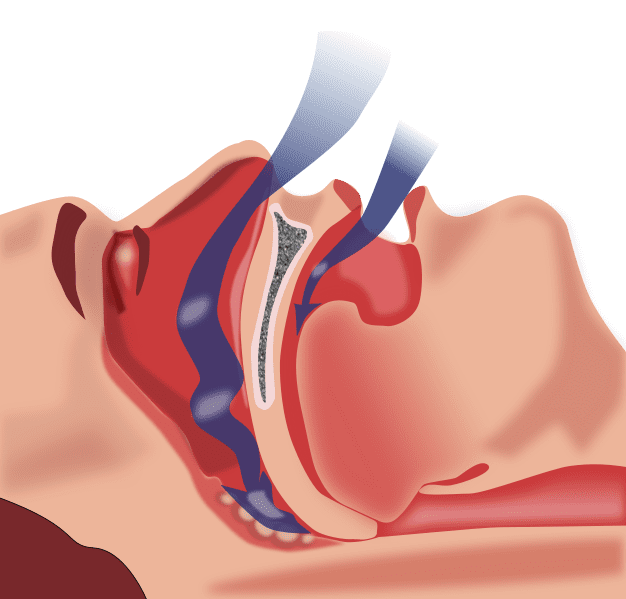
Obstructive sleep apnea (OSA) is caused by obstruction of the upper airway and is characterized by repetitive pauses in breathing during sleep, despite the effort to breathe. It is also usually associated with a reduction in blood oxygen saturation.
The study. All subjects underwent successful in-home sleep apnea studies and on-site audiometric testing at baseline.
Sleep apnea was assessed with the apnea-hypopnea index (AHI), which indicates sleep apnea severity based on the number of apnea (complete cessation of airflow) and hypopneas (partial cessation of airflow) per hour of sleep. Sleep apnea was defined as an AHI ? 15 events/hour.
High frequency hearing loss was defined as having a mean hearing threshold of greater than 25 dB in either ear at 2000, 3000, 4000, 6000 and 8000 Hz, and low frequency hearing loss was defined as having a mean hearing threshold of greater than 25 dB in either ear at 500 Hz and 1000 Hz.
Among the 13,967 study subjects, 9.9% had at least moderate sleep apnea (AHI ? 15), 19.0% had high frequency hearing impairment, 1.5% had low frequency hearing impairment, and 8.4% had both high and low frequency hearing impairment.
Hearing impairment was more common among individuals of Cuban and Puerto Rican descent and among those with a higher body mass index, self-reported snoring, and/or sleep apnea. Sleep apnea was independently associated with a 31% increase in high frequency hearing impairment, a 90% increase in low frequency hearing impairment, and a 38% increase in combined high and low frequency hearing impairment in analyses adjusting for age, sex, background, history of hearing impairment, external noise exposure, conductive hearing loss, and other factors. Increasing AHI was associated with a higher prevalence of high frequency, but not low frequency hearing impairment.
A limitation of this study was that the authors could not account for the impact of treatment of sleep apnea on their findings. However, it was rare for the participants to be on sleep apnea treatment in this cohort.
“Patients with sleep apnea are at increased risk for a number of comorbidities, including heart disease and diabetes, and our findings indicate that sleep apnea is also associated with an increased risk of hearing impairment” said Dr Chopra. “The mechanisms underlying this relationship merit further exploration. Potential pathways linking sleep apnea and hearing impairment may include adverse effects of sleep apnea on vascular supply to the cochlea via inflammation and vascular remodeling or noise trauma from snoring.”
In January 2012, The Hearing Review reported on a study from researchers in Taiwan who conducted a retrospective study that linked obstructive sleep apnea and subsequent diagnosis of sudden sensorineural hearing loss (SSNHL). In the February 2014 Hearing Review, Alessio & Marron also describe how vascular health and bloodflow can impact hearing status.
Source: ATS 2014