The groundbreaking work of Christine Yoshinaga-Itano et al1 in comparing the language abilities of earlier- and later-identified deaf and hard-of-hearing children has paved the way toward a universal goal of fitting hearing aids to children with hearing loss as early in life as possible. Dispensing audiologists refer these children to early intervention programs where they are often served by an educational audiologist who works for the program or the local school district.
Parents can become understandably confused when this additional audiologist makes a recommendation. Is this information to be delivered back to the dispensing audiologist who does the actual programming of the hearing aid? Is the parent the go-between? Should the two professionals talk to each other? Why multiple audiologists, anyway?
According to the American Academy of Audiology,2 “An audiologist is a person who, by virtue of academic degree, clinical training, and license to practice and/or professional credential, is uniquely qualified to provide a comprehensive array of professional services related to the prevention of hearing loss and the audiologic identification, assessment, diagnosis, and treatment of persons with impairment of auditory and vestibular function, and to the prevention of impairments associated with them. Audiologists serve in a number of roles including clinician, therapist, teacher, consultant, researcher and administrator.”
According to the Educational Audiology Association,3 in addition to “… perform[ing] complete hearing aid evaluations based on knowledge of current hearing aid options and prescriptive methods for selecting amplification characteristics,” educational audiologists are required to “… coordinate assessment and dispensing services between private agencies or professionals in the community and the school system.”
CHALLENGES IN FITTING CHILDREN
Catherine Palmer has written an excellent article in the Journal of Educational Audiology entitled “A Checklist/Protocol for Audiologists: Is This Hearing Aid Appropriate for This Individual?”4 In it, she proposes a test protocol whereby audiologists can evaluate whether hearing aid fitting goals have been met by an individual’s current hearing aids—regardless of whether they did the actual hearing aid programming themselves. Educational audiologists are often asked to answer this question by parents, and also work with teachers, speech-language pathologists, and other professionals whose treatment may be affected by the individual’s ability to hear. There also may be school guidelines that require annual evaluation of each child’s hearing aid.
While the reader is referred to Palmer’s article4 for more details, in summary, she describes several reasonable goals for any hearing aid fitting. They are “to make speech audible, comfortable, and to provide a good quality signal.”
Unfortunately, there is often disagreement within the audiological community about what gain values are needed to reach this objective. An informal poll of educational audiologists recently taken on the EdAud Internet listserv (July 2007) revealed that one of the most common sources of disagreement between educational audiologists and dispensing audiologists is a situation where a child’s fitting does not match desired targets, combined with poorer-than-expected speech and language development.
Requests to increase gain (particularly in the high frequencies) are often met with hesitation by dispensers. Pediatric audiologists most often use either the Desired Sensation Level (DSL) approach developed by Seewald and colleagues,5 or the revised National Acoustics Laboratories’ Nonlinear (NAL NL) procedure developed by that organization in Australia.6 Audiologists who focus on adult fittings may use one of those methods, or may prefer any of a number of other methods developed primarily for use with adults.
With the advent of programmable hearing aids, many audiologists and dispensers have come to trust the manufacturer’s software to integrate one of the accepted prescription procedures with the instrument’s particular processing strategies. So, one common approach is to enter all of the audiometric information into the software that programs the hearing aids, and let the automatic fitting take place.
However, recent studies tell us that this approach is not consistently accurate even for adult patients. David Hawkins and Jodi Cook7 showed that errors for adult-derived automated fittings existed, and were related to widely varying definitions of ear canal acoustics across manufacturers. They concluded that it was safe to assume that similar, or even greater, errors could occur for infants, and asked, “Should we be relying only on this for babies?”
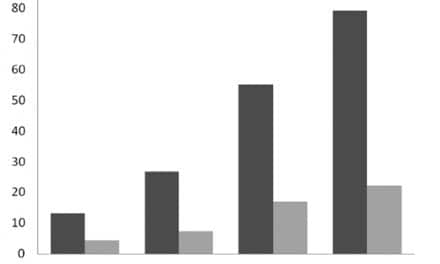
Richard Seewald, PhD, and colleagues8 took the question a step further. Fitting software from five manufacturers was evaluated, each selected because the company advertises its digital BTE hearing aids as being appropriate for pediatric applications. Nine theoretical audiograms, varying in degree and configuration of loss, were applied and assumed to belong to a 6-month-old child. They found that the majority of the generated prescriptions were suboptimal when compared to any evidence-based pediatric hearing aid prescription. Prescriptions varied by frequency and test level in terms of whether they over- or under-fitted. Frequency responses for speech varied in level and shape, and the results were different for soft versus average versus loud speech.
Even so, many audiologists will argue that their software-based methods are adequate, and some suggest that there shouldn’t be a difference between the gain that is appropriate for adults, and that needed for children. This may be changing, however, due to ideas propounded by Harvey Dillon, PhD (one of the developers of the NAL procedure, which may be the most widely used prescription procedure for adults). In it, Dillon states:
“… because children are still acquiring language, they are less able to use context. Therefore, they require more acoustic information than adults to understand speech and therefore require a different gain-frequency response. … Congenitally impaired children prefer more gain than adventitiously impaired adults, though the differences in gain do not appear to result in any differences in performance. Theoretically, an increased gain is most likely to lead to improved intelligibility at low input levels, so the child and adult versions of NAL-NL2 will be most different at low input levels. At these levels, there are no adverse safety implications from using a higher gain. …”6
WHAT TO DO? COMMUNICATION IS KEY
In view of these different philosophical backgrounds in fitting hearing instruments, how can professionals reach agreement on the appropriate amplification goals for a given child?
Communication is the key. The real answer is that each professional should establish and maintain relationships with the other professionals who are working with the family to develop the child’s communication skills. Most audiologists who work infrequently with children are eager to upgrade their skills, and a collegial relationship often involves sharing knowledge attained through continuing education.
Since many new tests have been added to the audiological protocol in recent years (see Auditory-Verbal International, 2003),9 it is often difficult to accomplish all desired evaluations in one session. Audiologists can collaborate to “fill in the blanks” in testing and save time and effort (eg, if one provider could obtain only air conduction thresholds, perhaps the other could test bone conduction, or high versus low frequencies, or right versus left ears). Clinicians doing auditory brainstem response (ABR) testing can do multiple frequency tone-burst testing that can then be used by a dispensing audiologist to fit the hearing aid.
Hearing aid verification and validation are an integral part of guidelines for pediatric hearing aid fitting,10 but they often are done infrequently, inadequately, or not at all. Not all audiologists have access to the necessary equipment, so this is another area where collaboration can be helpful. If one audiologist can make only measures of speech understanding, perhaps the other can do the real-ear measurements and speech mapping. Real-ear measurements should be made whenever the child gets new earmolds, as the acoustics may change considerably with the combination of new mold and ear size increase. If the earmold provider cannot do it, perhaps the collaborating audiologist can.
This is another area where communication with colleagues and trust in their results are crucial—by repeating some tests unnecessarily, we can end up defeating the fundamental goal of early identification and remediation. However, this kind of collaboration works only if testing is done in a timely manner, and if all parties have agreed upon amplification goals and methods. When done appropriately, it prevents overtesting and burnout in the child, and is a more efficient use of everyone’s time.
There are a number of areas where decisions need to be made about hearing aid settings and features. For example, use of directional microphones requires the listener to be looking at the speaker for optimum benefit—and how often does a 2-year-old look at the speaker?
Also, children need to be able to hear speech and environmental sounds that surround them in order to develop good communication skills. Although the evidence is conflicting in this area, many pediatric audiologists recommend omnidirectional microphones for children. Volume controls need to be disabled or covered until the child is old enough to be able to manipulate them. Tamper-resistant battery drawers are also important. Parents should be advised of these needs before they purchase the child’s hearing aids, as they are sometimes costly (or impossible) to alter after the fact.
Assistive technology can provide extraordinary benefit to children in overcoming the effects of poor classroom acoustics. Dispensers should be aware of the features and accessories needed (Direct Audio Input, FM-compatible boots, etc) and work with the educational audiologist to allow the child access to this technology.
Earmold technology is another area where adult-oriented audiologists often request assistance. This may change with the recent upswing in BTE fittings in adults, but clinicians’ knowledge about earmold acoustics is often underutilized, and conversations about acoustically tuned earmolds and soft earmold materials should be welcomed by both professionals.
Finally, input from parents, teachers, and therapists about auditory responsiveness and speech and language development can help to validate benefit. For example, a teacher’s report that a child responds to all Ling Sounds except /s/ and is having trouble with certain words may reveal a drop in high-frequency hearing or a need for fine-tuning of the hearing aid frequency response. Parents’ observations about their child’s shifting attention span may reveal an intermittent hearing aid or fluctuating hearing loss due to middle ear fluid.
Respect for parents—and for their observations about their children—is imperative. Parents know their children better than anyone and can provide helpful feedback to audiologists. Parents of children with hearing loss will vary in their responses to the diagnosis and in how they negotiate this new path in their lives.
It takes time for parents to assimilate the realities of their child’s hearing loss and to absorb new and technical information, especially when they are overwhelmed. Anxiety and depression can affect how parents respond to recommendations. Some parents may require more time than others to learn basic trouble-shooting and functional information about the hearing aids; others may educate themselves to the point that their questions can challenge even the most experienced audiologist. Encourage them all, and include them in all decision-making.
As David Luterman puts it:
“A persuasion model of counseling is not effective because the parent does not ‘own’ the decision and will blame others if the outcome is not successful. This model of counseling reinforces the parents’ feelings of inadequacy and tends to lead to passive, dependent parents waiting for professionals to tell them what to do.”11
Audiologists’ patience and their willingness to take the time to answer the parents’ many questions will forge strong and productive partnerships among educational and dispensing audiologists and parents.
Christine Gilmore Eubanks, PhD, is director of audiology at the John Tracy Clinic in Los Angeles. Correspondence can be addressed to [email protected].
REFERENCES
- Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL. Language of early- and later-identified children with hearing loss. Pediatrics. 1998;102:1161-1171.
- American Academy of Audiology. Audiology: Scope of Practice. McLean, Va: AAA; 2004.
- Educational Audiology Association. Recommended Professional Practices for Educational Audiology. Denver: EAA; 1997.
- Palmer C. A checklist/protocol for audiologists: is this hearing aid appropriate for this individual? J Educ Audiol. 2004;11:49-68.
- Seewald R, Moodie S, Scollie S, Bagatto M. The DSL Method for pediatric hearing instrument fitting: historical perspective and current issues. Trends Amplif. 2005;9(4):145-157.
- Dillon H. What’s new from NAL in hearing aid prescriptions? Hearing Journal. 2006;59(10):10-16.
- Hawkins D, Cook J. Hearing aid software predictive gain values: how accurate are they? Hearing Journal. 2003;56(7):26-34.
- Seewald R, Drake J, Scollie S, Sinclair-Moodie S, Bagatto M, Johnson A. A comparison of hearing instrument proprietary prescriptive procedures for infants with hearing loss. Paper presented at: American Academy of Audiology annual convention; April 2005; Washington, DC.
- Auditory-Verbal International. Suggested protocol for audiological and hearing aid evaluation. Available at: www.agbellacademy.org/Recommended_Protocol.htm. Alexandria, Va: AVI Publication; 2003.
- American Academy of Audiology. Pediatric Amplification Protocol. Audiology Today. 2004;16 (2):46-53.
- Luterman D. Counseling parents about cochlear implants. ASHA Leader. May 27, 2003;8:6-7, 20-21.