Back to Basics | March 2018 Hearing Review
As the name suggests, temporary threshold shift (TTS) is a temporary loss in sensitivity to certain sounds following an exposure to a loud noise or music. The pathophysiology is not well understood but appears to be, in part, related to the temporary disarticulation between the outer hair cells and the tectorial membrane in the cochlea (which re-establishes itself after 1-18 hours) and glutamate levels that become ototoxic, where the levels return to a normal (lower) level after 1-18 hours. This may be noted by the individual as a feeling of fullness or numbness after a loud event, with or without tinnitus, that can continue for several days after the event. TTS, being a “threshold” change, assesses cochlear pathology and is used as a measurement of such. Otoacoustic emission (OAE) testing also shows the temporary reduction in cochlear sensory function for a period after an exposure to noise or music. OAEs assess the function of the outer hair cells (efferently innervated) in the cochlea, so TTS is considered to be a cochlear dysfunction.
TTS Pre- and Post-2000
Prior to the year 2000, TTS was considered to be a benign feature of exposure to noise or music, resolving in 1-18 hours—a temporary cochlear phenomenon. Because TTS was “temporary,” it was a paradigm commonly used to assess whether a person was subjected to an overly high level of noise or music. Academic research review boards have little concern with approving such studies. Therefore, much of the research revolved around whether a measure of TTS could be used to predict future permanent threshold shift (PTS). However, no research has shown that TTS (or the pattern of recovery from TTS) can be used as a predictor of future PTS. I have to admit that, in the 1980s and 1990s, when a client came in with symptoms of TTS, I was rather dismissive.
Since the year 2000, a number of studies have demonstrated that, despite hearing thresholds returning to the pre-exposure level (ie, no measureable TTS), there can be some permanent neural deficits that may not be immediately detectable. That is, despite a return to normal cochlear function (with a normal audiogram), the neural deficits may remain. Specifically, the synapse from the cochlear inner hair cells (afferently innervated) to the VIII auditory nerve can be permanently altered with a reduced amplitude on the Wave I on a traditional ABR-evoked audiometry paradigm. This has been referred to as “cochlear synaptopathy.”1-4 There are currently no accurate measures of cochlear synaptopathy and its prevalence is not well-defined, although there have been some recent attempts to use envelope following responses (EFRs) to AM tones.5
While prevalence estimates of cochlear synaptopathy in animal models are found in the literature, it may be erroneous to relate this to humans. There is very little data but there has been some research on human temporal bones. Viana et al6 counted the number of synapses in five temporal bones. As a function of age, there were fewer synaptic connections at the time of death. Another study by Makary et al7 showed that, again, as a function of age in 100 human temporal bones, there was a marked decrease in cochlear spiral ganglion cells, despite having intact cochlear sensory cell populations at the time of death.
Cochlear synaptopathy has colloquially been referred to in the media as “hidden hearing loss,” and while that can grab headlines, at this point in time little is known about how this can manifest itself in humans, how this can be reliably measured, and what the prevalence actually is.
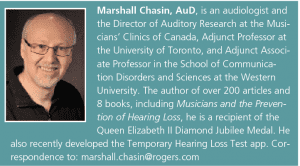
Original citation for this article: Chasin M. Changes in thinking about TTS: Pre- and post-2000. Hearing Review. 2018;25(3):10.
Image: © Voyagerix | Dreamstime
References
-
Kujawa SG, Liberman MC. Adding insult to injury: Cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci. 2009;29(45)[November]:14077-14085.
-
Kujawa SG. Putting the ‘neural’ back in sensorineural: Primary cochlear neurodegeneration in noise and aging. Hear Jour. 2014;67(11)[November].
-
Kujawa SG, Liberman MC. Synaptopathy in the noise-exposed and aging cochlea: Primary neural degeneration in acquired sensorineural hearing loss. Hear Res. 2015;330(B)[December]:191-199.
-
Liberman MC, Kujawa SG. Cochlear synaptopathy in acquired sensorineural hearing loss: Manifestations and mechanisms. Hearing Res. 2017;349[June]:138-147.
-
Paul BT, Waheed S, Bruce IC, Roberts, LE. Subcortical amplitude modulation encoding deficits suggest evidence of cochlear synaptopathy in normal-hearing 18–19 year olds with higher lifetime noise exposure. J Acoust Soc Am. 2017;142(5):EL434.
-
Viana LM, O’Malley JT, Burgess BJ, et al. Cochlear neuropathy in human presbycusis: Confocal analysis of hidden hearing loss in post-mortem tissue. Hear Res. 2015;327[September]:78-88.
-
Makary CA, Shin J, Kujawa SG, Liberman MC, Merchant SN. Age-related primary cochlear neuronal degeneration in human temporal bones. J Assoc Res Otolaryngol. 2011;12(6)[December]:711-717.