Amplification options for patients with steeply sloping sensorineural hearing loss (SNHL in excess of 50 dB/octave) are fairly limited. Patients with precipitous high-frequency SNHL represent a significant challenge for hearing care professionals. In the majority of cases, they do not meet the requirements for cochlear implant candidacy, but they are often dissatisfied with hearing aid performance. Yet, there is little doubt that low-frequency acoustic amplification preserves temporal information that is important for speech recognition in noise and sound quality.
Apart from traditional amplification, other strategies include open fittings and frequency transposition (discussed below). Cochlear implant/hearing aid hybrids that combine acoustic and electric hearing offer significant potential for this population, but the “invasive” nature of the implant procedure is likely to represent an obstacle to their widespread acceptance.

|
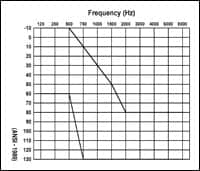
| FIGURE 1. Fitting range for patients with “steeply-sloping losses” who are potential candidates for open hearing aid fittings and/or hybrid cochlear implants. (click image for larger view.) |
The number of patients with steeply sloping SNHL—a hearing loss that may arise from noise exposure, presbycusis, and ototoxicity, or combinations of these factors—is expected to increase as the global “baby boom” generation (people born from 1946-1964) ages. In the United States, there are 77 million Baby Boomers, and many have acquired hearing loss due to a combination of occupational and non-occupational noise exposure. It is hard to pinpoint exactly how many patients have steeply-sloping losses (Figure 1), but it is estimated that many are not wearing conventional amplification due to stigma, lack of perceived benefits, and/or cost.2
In recent years, new technology has been developed to focus specifically on the needs of patients with these types of hearing losses.
Open-Fit Hearing Aids
Although not a new concept, “open-fit” hearing aids have enjoyed a renaissance in popularity during the past few years. Since 2005, most major hearing aid manufacturers have offered open-fit aids that are either specifically developed for open fittings or modified from existing product families. Effective open-fit strategies comprise:
1) Minimal occlusion via a narrow (0.8 mm) tube fitting or large vented earmold (>3.0 mm diameter);

|
| FIGURE 2. Vent parameters for different parallel vent diameters and for an open “tube” fitting with no canal occlusion. Based on Lybarger (1985).1 (click image for larger view.) |
2) Feedback phase cancellation system;
3) Minimal signal processing group delays (<15 ms);
4) Precise frequency compensation with steep filter slopes; and
5) Directional microphones to improve speech recognition in noise.
The last factor, directional microphones, has repeatedly been proven to be the single factor most related to patient satisfaction and benefit with hearing aids. Conventional wisdom, however, has suggested that open fittings and directional microphones are mutually exclusive. This is due primarily to the idea that the acoustic properties of venting act to attenuate low-frequency gain (below 1000-1500 Hz), where directional microphones are most effective. This is illustrated in Figure 2 (above right), which is based on work conducted by Lybarger in the mid-1980s.1

|
| FIGURE 3. Prototype directional microphones system with 5 mm microphone spacing between microphone ports. (click image for larger view.) |
Modern directional microphone systems have been developed that preserve directional benefits for frequencies in excess of 6000 Hz by placing the microphones closer together than in the past. The previous industry standard separation used in hearing aids was 12 mm, which limited directional benefits to below approximately 4000 Hz. An example of a system that uses a separation of 5 mm between microphones is illustrated in Figure 3. Although hearing aid internal noise is lower with the wider separation, these new digital hearing aids eliminate that issue by using “acoustic scene analysis” to automatically monitor the listening environment and activate either omni-directional or directional microphones when appropriate. As a result, considerable directional benefits (in excess of 6 dB) will still be achieved for frequencies between 1500-6000 Hz when the system is coupled to an open-fit device (Figure 3). This translates into measured speech recognition improvements in noise of 20-30% (ie, 2-3 dB SNR benefit) over comparable open-fit hearing aids with omni-directional microphones.
Of course, feedback phase inversion is essential in order to enable these high-frequency components of speech to be amplified without producing feedback oscillation. It is also crucial that the patient have adequate residual hearing to take advantage of these high-frequency cues.
High-Frequency Hearing Loss and Auditory “Dead Regions”
Identification of the distortion effects inherent with precipitous hearing loss date back many years.3 Lately, Moore4 has coined the term “auditory dead regions” to characterize those patients who have regions in the cochlea where there is no transduction of basilar membrane motion in specific regions due to missing or damaged inner hair cells (IHCs). Although “dead regions” may exist anywhere along the cochlear partition, they tend to be more prevalent in people with precipitous high-frequency hearing losses. As such, despite the improvements in open-fit devices to deliver more high-frequency amplification to the ear without feedback, the distortion effects caused by hearing loss may prevent users from benefiting from this improved audibility.
Several investigators5,6 have indicated that there is an inverse relationship between sound pressure level (SPL) and word/ phoneme recognition level for SPLs above typical conversational speech levels. In other words, for fixed SNRs, performance degrades with increases in presentation level. Although this relationship exists for both normal-hearing and hard-of-hearing people, it is more pronounced in patients who have severe-to-profound hearing loss. Specifically, increased audibility does not translate into improved speech understanding, in quiet or in noise, when damage exceeds moderate-to-severe SNHL.
The bottom line is that—if psychophysical tuning curves (PTCs), speech recognition, or residual dynamic range are abnormal—open fittings (or any acoustic amplification strategies) may be of little use in those frequency regions.
Frequency Compression
Frequency compression is another amplification strategy for high-frequency hearing losses that has been available but used rarely until recent years. There are a wide variety of techniques that may be used,7,8 but the main objective is to shift high-frequency information to lower frequency regions where there are surviving inner (and possibly outer) hair cells. Theoretically, this approach may provide an amplification solution for patients with “auditory dead regions” by providing audibility for high-frequency speech cues by enabling transduction of this transposed information into basilar membrane motion.
To date, however, frequency compression has proven to be effective in only half of the patients who try it8 due to their inability to “remap” the way high-frequency sound is perceived when it shifts to another frequency region. This may be due, in part, to frequency compression thresholds and ratios being set too low and too high, respectively, and warrants further investigation. Regardless, frequency compression, in combination with open fittings and directional microphones, may serve as an appropriate non-invasive amplification benchmark prior to implantation.
Summary
Hearing aid technology has improved dramatically in recent years. In the United States, roughly 90% of all hearing aids dispensed in 2006 were digital, offering improved fitting flexibility, feedback reduction, and multichannel compression strategies to ensure audibility for soft, moderate, and loud sounds. Open-fitting platforms have regained in popularity, due primarily to this improved fitting flexibility in combination with feedback phase inversion systems that may be used to dynamically cancel hearing aid feedback.
For patients with steeply-sloping SNHL, however, this improved technology may not be effective, due to reduced dynamic range and increased distortion that accompanies peripheral loss. In extreme cases, “auditory dead regions” may prevent the transduction of basilar membrane motion on specific regions of the cochlea. For these patients, it’s possible that future combined electric-acoustic hearing aids provide a solution, but the invasive nature of the treatment may limit popularity of these hybrid devices. Prior to making the surgical decision, patients should be fit with a state-of-the-art open-fit or frequency compression device to make certain that they cannot benefit significantly from acoustic hearing aids.
Finally, preliminary data suggest that preservation of acoustic hearing, even for very low-frequency sounds, provides improved speech recognition in noise and sound quality versus unimodal stimulation via electric or acoustic-only stimulation in these patients.
References
- Lybarger S. Earmolds. In: Katz J, ed. Handbook of Clinical Audiology. 3rd edition. Baltimore: Williams and Wilkins; 1985:885-910.
- Kochkin S. MarkeTrak VII: Hearing loss population tops 31 million people. The Hearing Review. 2005;12(7):16-29.
- Plomp R. A signal-to-noise ratio for the speech reception threshold of the hearing impaired. J Speech Hear Res. 1986;29(2):146-154.
- Moore BC. Dead regions in the cochlea: Conceptual foundations, diagnosis, and clinical applications. Ear Hear. 2004;25(2):98-116.
- Studebaker GA, Sherbecoe RL, McDaniel DM, Gwaltney CA. Monosyllabic word recognition at higher-than-normal speech and noise levels. J Acoust Soc Am. 1999;105(4):2431-2444.
- Hornsby BW, Trine TD, Ohde RN. The effects of high presentation levels on consonant feature transmission. J Acoust Soc Am. 2005;118:1719-1723.
- Turner CW, Hurtig RR. Proportional frequency compression of speech for listeners with sensorineural hearing loss. J Acoust Soc Am. 1999;106(2):877-886.
- Simpson A, Hersbach AA, McDermott HJ. Improvements in speech perception with an experimental nonlinear frequency compression hearing device. Intl J Audiol. 2005;44(5):281-292.
Correspondence can be addressed to HR or David Fabry, Phonak Hearing Systems, 4520 Weaver Parkway, Warrenville, IL 60555; e-mail: .