Patient success hinges on conversation intelligibility and repair by all talkers
Everyday conversation is at the heart of living well, and its successful conduct is critical to one’s image as a competent social being. All conversation may be judged by the way participants are able to take responsibility toward mutually successful interaction; living well with hearing loss is influenced by the way all people in various conversations play their part. Therefore, the success of any conversationally oriented rehabilitation program should focus on both speaker intelligibility and conversation repair.
The ability to successfully converse with others is critical to one’s image as a competent human being and impacts one’s perceptions of happiness or living well in society. All conversation may be judged by the way participants are able to take responsibility toward mutually successful interaction, and living well with a hearing loss will be influenced by the way all people in the conversation play their part.
Adults who have acquired hearing impairment (HI) commonly report difficulties in everyday conversation, and as such, amelioration of these difficulties is a legitimate goal of intervention for audiologists and other hearing care professionals. The success of a clinical intervention may be judged by the success hearing-impaired adults and their partners perceive in everyday conversation.

Christopher Lind, PhD, is a senior lecturer in audiology at Flinders University, South Australia.
This article discusses how clinicians can gain insight into both the way hearing-impaired adults communicate with their partners and how this might influence their perceptions of living well.
Living Well: Conversation and Acquired Hearing Impairment
How one might live well has been the focus of philosophical debate for centuries. Philosophical perspectives on living well, or perhaps “happiness,” started with Greek philosophy: the Epicureans’ meeting of (modest) material needs, the Hedonists’ avoidance of pain and the seeking of pleasure, or the Stoics’ search for goodness and virtue, for example. Later philosophical ideals include Hume’s model of self-worth and good character and Mill’s exercise of free will. Of course, these are but a few perspectives and there are many other philosophical views and interpretations one might take (eg, Kenny1).
In each case, however, living well is embedded in a social milieu, and implies one’s ability to participate in society in order to meet these ideals. We might each see a little of ourselves in each philosophy. Indeed, the ideal of living well underpins much of our daily activity while it seems to be a concept to which we pay little overt attention until it is compromised.
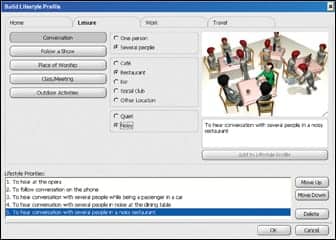
The premise of this brief paper, and indeed of the Ida Institute’s Living Well with Hearing Loss seminars (2010-2011), is that there is the potential for acquired HI to threaten one’s ability to live well. As such, “living well” may be a valid goal of rehabilitation services for adults with HI, their families, and friends. This paper focuses on one element of this potential threat and the clinical response to it—namely, the relationship between living well, HI, and successful everyday spoken conversation.
Implications of Conversational Difficulties
While most adults participate in conversation every day of their lives, the concept of success in conversation is largely taken for granted. Most of us have been conversing successfully since our second year, and some might say from even younger.2,3 We interact in order to participate in life’s activities; to become someone; to develop a social identity.4,5 In doing so, we have been able to establish that the people we talk to understand us and that we understand them. We have been able to respond to brief interruptions, misunderstandings, or other acts that interfere with the flow of conversation readily and efficiently since we were 4 or 5 years old.6
This is not always the case for many adults in the community who have acquired HI. Disruption or even cessation of everyday conversation is the most disabling consequence of acquired HI,7 leading to adverse effects on the HI individual’s self-image, psychological health, and social participation.8
Consequences of HI during conversations. In order to consider how acquired HI threatens one’s ability to live well as a result of a loss of conversational success, we need to ask what successful conversation might be in the first place. Might it be equated with fluency (ie, the flow of conversation including few long pauses, few overlaps, and relatively few stops and starts), ease (ie, the perceptions associated with conversation are those of relaxed and effortless talk), enjoyment of the content (ie, attitudes toward the interest or stimulation of a particular topic of discussion), or the social contact it awards one, for instance? Or might it be based on something else? There is little consensus on this question, and the answer may vary from conversation to conversation.
It is clear that conversations involving adults who have acquired HI are marked by an increased likelihood of certain types of breakdown and repair,9,10 avoidance of talk,11 and increased number of monologues by the HI adult.12 They also demonstrate more topic changes and less topic elaboration/discussion,13 shorter turns with less semantic content,14 and an increased use of general fillers and back-channeling.13
Any or all of these may influence perceptions of conversational success (and by extension, living well) by the HI adult. Importantly, these perceptions may also arise for the communication partner.15 So how might clinicians address perceptions of reduced conversational success by the HI client and/or by their communication partner during the brief period that they have with their clients—particularly in rehabilitative clinical settings?
Intelligibility and Repair: Addressing Conversational Problems in the Clinic
Traditionally, audiologists have offered speech reception training as the major model of rehabilitation under the reasonable (but largely tacit) premise that the HI client’s otherwise adequate communication skills are compromised solely by the loss of auditory access to another’s speech. As a result, improvements in reception may be achieved via hearing aid fitting and by audiovisual speech reception (or more usually, “speechreading”) skills. However, the question remains how clinicians might place these (and possibly other intervention strategies) into a conversational context if it is agreed that improvements in everyday conversation are the goals for many of our adult clients.
First, we can put a conversational slant on audiovisual speech reception by replacing the concept of speechreading (ie, an act the HI adult undertakes) with the concept of intelligibility (an interactive/shared undertaking). If we view conversation as an activity that always involves another, then it is not remarkable that those who communicate regularly with HI adults carry some of the burden of the difficulties that might arise.9,10 By extension, they may also be able to alleviate some of the difficulties by their use of targeted communication strategies (for example, see Erber,16 Kaplan et al,17 and Pedley et al18).
Research guides us as to how we might engage the communication partner to develop strategies that improve their communication with their HI partners, family members, friends, workmates, etc. We know that talkers vary in the clarity/intelligibility of their speech,19,20 and that there is a substantial difference between clear and conversational speech.21,22 We also know that communicators are able to improve the intelligibility of their speech on demand from their communication partner.23 They are also able to spontaneously alter their speech proportionally to the increase in distance from the listener24 and in response to perceived changes in the complexity of the text they are reading25—in both cases, without instruction.
Second, despite participants’ best efforts at making their turns in conversation sufficiently clear for their communication partner, there are times in a conversation when miscommunication occurs.9,10 While these are everyday events for all of us (of which we typically remember almost nothing), their frequent occurrence—and the time taken to resolve them—potentially causes HI adults to shy away from conversation and fear the perception of failure or incompetence that this implies.
It should be emphasized that conversation breakdown (and its subsequent repair) is commonplace, familiar, and unremarkable. Even though it may be the case that the person asking for clarification has a HI, there is seldom direct or clear evidence that the repair is caused by the HI. Breakdown is better seen as a self-righting mechanism than as an error by one or the other speaker.26
When observing conversation in the clinic (or indeed, anywhere), we might expect that:
- Repairs will occur, maybe quite often;
- They are resolved easily; and
- Both partners participate in their resolution.
We should make it clear to our clients that neither partner should apportion blame for the miscommunication. However, it is a goal for future therapy models in aural rehabilitation to alleviate the burden on HI adults and their partners that those frequent miscommunications and/or long sequences of turns in repair might impose.
Conversation-based intervention is based on the premise that HI adults and their communication partners will benefit from bringing under their conscious control aspects of everyday interaction that are (or will potentially be) adversely affected by the HI. Further, two complementary elements in this therapy model may assist in lessening the effects of acquired HI on everyday conversation: intelligibility and repair.
We have sufficient research to develop clinical activities to address these two topics with our clients. Structured clinical practice in the former may reduce the likelihood of miscommunication and in the latter may reduce time spent in repair. Both are valid and important communication goals.
Summary
Everyday conversation is at the heart of living well, and its successful conduct is critical to one’s image as a competent (and happy) social being. Clinical interactions give insight into both the content/ideas and process/sequences of HI adults’ communication with their partners. All conversation may be judged by the way participants are able to take responsibility toward mutually successful interaction, and living well with HI will be influenced by the way all people in the conversations play their part.
Conversationally oriented rehabilitation programs may focus on both speaker intelligibility and repair. The success of intervention may be judged ultimately by the success HI adults and their partners perceive that they have in everyday conversation. In turn, this success might influence one’s perceptions of living well.
References
- Kenny A. A New History of Western Philosophy. New York: Oxford University Press; 2007.
- Berko Gleason J. The Development of Language. 5th ed. Boston: Allyn & Bacon; 2001.
- Paul R. Language Disorders from Infancy Through Adolescence. 3rd ed. St Louis: Mosby/Elsevier; 2007.
- Berk LE. Child Development. 6th ed. Boston: Ally & Bacon; 2003.
- Hoff E. Language Development. 3rd ed. Belmont, Calif: Cengage Learning; 2005.
- Brinton B, Fujiki M. Responses to requests for conversational repair by adults with mental retardation. J Speech Hear Res. 1991;34:1087-1095.
- Stephens D, Gianopoulos I, Kerr P. Determination and classification of the problems experienced by hearing-impaired elderly people. Audiology. 2001;40:294-300.
- Heine C, Browning CJ. The communication and psychosocial perceptions of older adults with sensory loss: a qualitative study. Aging and Society. 2004;24:113-130.
- Lind C, Hickson L, Erber NP. Conversation repair and acquired hearing impairment: a preliminary quantitative clinical study. J Aust N Z Audiol Soc. 2004;26:40-52.
- Lind C, Hickson L, Erber N. Conversation repair and adult cochlear implantation: a qualitative case study. Cochlear Implants Intl. 2006;7:33-48.
- Stephens SDG, Jaworski A, Lewis PA, Aslan S. An analysis of the communication tactics used by hearing-impaired adults. Brit J Audiol. 1999;33:17-27.
- Wilson J, Hickson L, Worrall L. Use of communication strategies by adults with hearing impairment. Asia Pac J Speech Lang Hear. 1998;3:29-41.
- Pichora-Fuller MK, Johnson CE, Roodenburg KEJ. The discrepancy between hearing impairment and handicap in the elderly: balancing transaction and interaction in conversation. J Appl Commun Res. 1998;26(1):99-119.
- Johnson CE, Pichora-Fuller MK. How communication goals may alter handicap. J Speech Lang Pathol Audiol. 1994;18:235-242.
- Scarinci N, Worrall L, Hickson L. The effect of hearing impairment in older people on the spouse. Int J Audiol. 2008;47(3):141-151.
- Erber NP. Hearing, Vision, Communication and Older People. Melbourne: Clavis; 2002.
- Kaplan H, Bally SJ, Garretson C. Speechreading: A Way to Improve Understanding. Washington, DC: Gallaudet University; 1985.
- Pedley K, Giles E, Hogan A. Adult Cochlear Implant Rehabilitation. London: Whurr; 2005.
- Kricos PB, Lesner A. Differences in visual intelligibility across talkers. Volta Review. 1982;84:219-225.
- Kricos PB, Lesner A. Effect of talker differences on the speechreading of hearing impaired teenagers. Volta Review. 1985;87:5-16.
- Picheny MA, Durlach NI, Braida LD. Speaking clearly for the hard of hearing, I: Intelligibility differences between clear and conversational speech. J Speech Hear Res. 1985;28:96-103.
- Picheny MA, Durlach NI, Braida LD. Speaking clearly for the hard of hearing, II: Acoustic characteristics of clear and conversational speech. J Speech Hear Res. 1986;29:434-446.
- Schum DJ. Intelligibility of clear and conversational speech of young and elderly talkers. J Am Acad Audiol. 1996;7:212-218.
- Michael D, Siegel G, Pick H. Effects of distance on vocal intensity. J Speech Hear Res. 1995;38:1176–1183.
- Pedlow R, Wales R. Some effects of context on spoken language production. Language and Speech. 1987;30:373-385.
- Schegloff EA, Jefferson G, Sacks H. The preference for self-correction in the organization of repair for conversation. Language. 1977;53:361-382.
Correspondence can be addressed to HR or Christopher Lind, PhD, at .
Citation for this article:
Lind, C. Living Well: Everyday Conversation and Hearing Impairment Hearing Review. 2011;18(8):24-26.