Abundant evidence indicates that every hearing aid dispensed should feature a directional microphone. Yet, only 20% to 30% of all hearing aids do. Why? One reason is that as few as 8% of dispensing professionals have access to the QuickSIN or HINT tests, and perhaps even fewer realize that half of their patients are leaving their offices with a 5 dB signal-to-noise ratio (SNR) hearing loss. In this context, it’s no wonder that some users continue to complain, “I hear better without my hearing aids.” Additionally some directional systems offer relatively low (<2 dB SNR) improvement in noise. Although it’s important to recognize that even these small increases in SNR can lead to significantly better hearing in noise, an AI-DI improvement of less than 2 dB is unlikely to be noticed by patients in most listening environments.
As mentioned in Part 11 of this three-part series of articles, the motivation for the following reflections comes partly from three MarkeTrak studies published in HR by Sergei Kochkin2-4 which report:
- 80% of those who admit they need hearing aids don’t buy them;
- 40% of those who do buy hearing aids do not place themselves in the “satisfied” category;
- Better understanding of speech in noise is the largest improvement sought by those wearing hearing aids; and
- Improved sound quality is the second largest improvement sought by those wearing hearing aids.
There are good reasons to recommend directional microphones with every hearing aid. This is supported by four premises:
- Directional microphones provide the only verified method of improving the ability of hearing aid users to understand speech in noise. Noise-reduction circuits do not.
- The cost of adding high-performance directional microphones is trivial compared to the cost of today’s digital hearing aids.
- A surprising number of times normal-hearing patients complain that “hearing in noise” is their biggest problem, even though they have a normal audiogram and test within normal limits for hearing in noise on the QuickSIN test (this has been noted by several clinicians, including correspondence with David Hawkins, PhD, Mayo Clinic, Ft. Lauderdale).
- There is a stigma attached to wearing hearing aids.
Can We Reduce Stigma by Using Directional Hearing Aids?
The fourth item requires discussion. In lectures, Edgar Villchur has speculated that the reason hearing aids have a large stigma and eyeglasses have little stigma may be simply that hearing aids don’t always work well; specifically, they don’t solve the real problem of hearing in noise. When we see someone wearing eyeglasses, we assume they can see quite well in all situations. Conversely, when we see someone wearing hearing aids, experience tells us that they probably don’t hear well, and that they may not be able to keep up with conversation in a restaurant or at a party. A stranger may even wonder if their comprehension is impaired. It is precisely those situations in which wearers are readily observed that loss of the ability to hear in noise often substantially exceeds any correction supplied by the hearing aid.
Unfortunately, only 20% to 30% of dispensing professionals obtain directional-microphone hearing aids for their patients.3,5 In many cases, directional microphones are reserved for patients with the greatest signal-to-noise ratio (SNR) losses, so those patients are still coping with a substantial SNR loss even after benefiting from the directivity of the hearing aids. On the other hand, most dispensing professionals do recommend the use of hearing aids that feature digital noise reduction. To our knowledge, no one has proved that a digital noise reduction scheme improves the ability to understand speech in noise over and above the improved understanding provided by signal processing that makes more speech cues audible. As long as nearly every hearing aid wearer is left with obvious difficulty hearing in noise, we can speculate that the stigma will continue.
But what if all patients with less than 5 dB SNR loss were fitted with good hearing aids that included directional microphones having AI-DI performance of 5 dB or better? Many of those patients would then be able to understand speech better than their normal-hearing companions at a restaurant or noisy party. The 20% with little or no SNR loss would be able to understand conversations even when the SNR was 3 dB to 5 dB worse than their normal-hearing companions could tolerate (a 3 dB SNR increase corresponds to about 30% increase in sentence scores). At the least, we would begin to erase the stigma associated with wearing hearing aids.
Myth: Measurable Benefit Equals Noticeable Benefit
There is a pitfall in this suggestion, however. Evidence discussed in this article suggests that the real-world directivity of some ITE hearing aids is so low that switching from an omnidirectional (omni) setting to a directional setting will not provide a noticeable increase in intelligibility.
Anecdotally, in perhaps 500 hours of testing and wearing directional-microphone hearing aids over the years (starting in the 1970s), the author has observed that, when using array microphones with over 7 dB AI-DI directivity, the improved performance in noise is almost always immediately obvious. With directional microphones having 4-5 dB real-ear AI-DI, the improvement is usually heard readily on the first comparison in restaurants and cocktail parties, but this is not always true. Even with 4-5 dB AI-DI, there are times when the moment-to-moment variations in noise and talker level are great enough that the improvement is not obvious without two or three back-and-forth comparisons. For example, the background might swell up just after switching to the directional mode, making it seem as if the directional mode was worse.
What if there is an amount of directivity that can rarely be detected in a real-world environment? And what if the directional performance of many hearing aids fall below this number?
Among other things, this might help explain the results of Walden et al.,6 whose 40 subjects reported an average improvement of only 3% (0.3 on a 0-10 scale) in real-world performance when comparing directional and omni microphone modes (using a scale in which 0 equalled “very poor” and 10 equalled “very good”). The estimated AI-DI of the aids they used was 1.9 dB. Author’s Note: Walden et al.6 found average improvements in sentence scores at 60 dB and 75 dB SPL of 20% and 32% respectively between directional and omni microphone settings in a test booth. We can estimate the directivity of the hearing aids they used based on the slope of 13.8%/dB Cox et al.7 reported for the CST: The 20% and 32% test-booth differences in speech-in-babble scores suggest differences of 1.5 and 2.4 dB SNR, respectively, or an average of 1.95 dB apparent SNR improvement in their test booth condition. In fact, the actual AI-DI performance may have been even less: Given the time delay of 0.8 ms across the head, the results of Julstrom8 suggest we may treat the noise from the three speakers as uncorrelated, so the loudspeaker arrangement used in that experiment (noise sources at 90°, 180°, and 270°) would have provided an SNR improvement significantly larger than the actual AI-DI rating. Rather than make an uncertain correction, an AI-DI estimate of 1.9 dB is used here.
So, What Is the Minimum Detectable Directivity Improvement Limit?
What AI-DI performance is so small that hearing aid users won’t be able to reliably hear the difference in a real-world listening environment? The question is important because many available directional-microphone hearing aids have AI-DI directivity of 3 dB or less, especially after venting.
Minimum detectable differences have been established for various characteristics of sound, but we are not aware of any measure of minimum detectable differences in SNR under real-life or simulated real-life conditions. We thus created a Minimum Detectable Directivity Improvement (MDDI) test to simulate the case in which a hearing aid wearer in a noisy restaurant or social situation switches back and forth from omni to directional mode and tries to hear the improvement, if any, in the directional mode. We adjusted the level of the talker in the separate-tracks section of the QuickSIN test,9 and asked subjects to make A-B comparisons between presentations in which the talker-to-babble ratio in B relative to A was randomly varied in 2-dB steps from -6 dB to +6 dB SNR. The QuickSIN segments were chosen because the talker/babble SNR had already been made equivalent across sentences during its development.
Figure 1A.
Figure 1B.
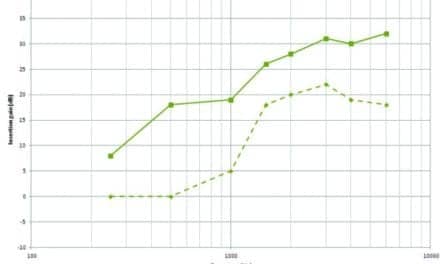
Figure 1A-B. Detection of SNR differences in 16 subjects when using a female talker with 4-talker babble. 1a) Average judged SNR vs. presented SNR; 1b) Percent correct identification of SNR differences vs. actual SNR differences.
The results shown in Figure 1a indicate that the listening test itself is reasonably accurate on the average, but that in identifying SNR differences, subjects operate at only chance performance for a 2 dB difference between omni and directional AI-DI.
.gif)
Besides Walden et al.,6 at least three other studies10-12 since 1995 have reported directional benefit—as indicated by subject responses on the Background Noise (BN) subscale of the Profile of Hearing Aid Benefit13—using directional microphones in which the AI-DI was reported or could be estimated from the available data. Figure 2 shows the relationship between reported benefit and estimated AI-DI for all four studies, data that tend to support the conclusion that an AI-DI greater than 2 dB is required for significant perceived benefit.
This is not to say that an AI-DI of 2 dB (or even less) is not valuable to patients. For example, patients obtained 20% and 32% increased sentence scores in the directional mode in Walden’s soundbooth experiments.6 Thus, even relatively small increases in SNR improvement can lead to significantly better hearing in noise; however, an AI-DI as low as 2 dB is unlikely to be noticed by the patient in a real-world setting.
The Importance of Measuring the Patient’s SNR Loss
We have sometimes been content to “do our best” in fitting hearing aids, even when the result leaves a moderate-to-severe handicap for hearing in noise. Unfortunately, the “best we can do” without adequate information is not always sufficient. When dispensing professionals don’t measure the degree of hearing loss in noise—the SNR loss—that their patients have, there is no way to determine the extent of the problem the patients are left with when they leave the office. According to Mueller,14 only 8% of dispensers appear to regularly use a HINT or QuickSIN test, the two popular tests for measuring SNR loss. The HR Dispenser Survey5 indicated that about 2-in-5 offices (42%) reported routine conducting of speech-in-noise testing using the SIN, QuickSIN, HINT, or some other method.
Thus, the reason that 70% to 80% of patients leave the office without directional microphones is probably because few dispensing professionals realize that half of all their patients have an SNR loss of 5 dB or greater. In most cases, ignorance is not bliss—nor does it bode well for customer satisfaction. Indeed, the above may be the explanation for why otherwise good dispensing professionals are not succeeding in providing the help their patients need for hearing in noise. Just as importantly, knowing the patient’s SNR loss allows the dispensing professional to counsel their patients about the problems to expect in noise (even accounting for the benefits of directionality), so that patients with moderate SNR loss who read the glowing brochures will not experience disappointment.
.gif)
Figure 3 shows the SNR loss-distribution data gathered from Cannito & Taylor,15 Arcaroli,16 and dispensing sites in Illinois, Florida, and California (unpublished data, D. Benson & D. Hawkins’ 2001 survey of SNR distribution for hearing aid patients, and M.C. Chisolm, P. Pessis & G. Gudmundsen’s 2000 survey of 150 hearing aid patients analyzed for SNR in three audiology practices). The study showing the greatest average SNR loss was the Cannito & Taylor study.15 We asked if we could retest a random sample of 15 of patients from this study, and the researchers readily agreed. We actually found slightly higher SNR losses on retest of most of his patients; the researchers had reported the better of two QuickSIN scores and we reported the average. The combined data indicate that approximately 50% of hearing aid wearers have an SNR loss of 5 dB or greater, and 20% have an SNR loss of 10 dB or greater.
It is also interesting to note the exceptional improvement in cochlear implant processors. At one time, only the cochlear implant “stars” could carry on a conversation without lipreading. Of the group of 19 recent cochlear implant patients in the Arcaroli study16 (Figure 3), 1-in-7 (those with less than 12 dB SNR loss) would understand speech in noise better than 15% of hearing aid wearers. If those same cochlear implant patients could make use of a good directional microphone (eg, a 5 dB AI-DI directional microphone, effectively reducing a 12 dB SNR loss to a 7 dB SNR loss) and the hearing aid wearers did not, the best of the cochlear implant patients would hear better in noise than 40% of the hearing aid wearers!
More to the point, consider that the addition of good directional microphones (Ž5 dB AI-DI) to the better hearing aids would mean that 50% of hearing aid wearers should be able to understand speech in noise at the same SNR as the average normal-hearing subject, assuming the noise is typical of restaurants and social gatherings (where the noise arrives with more or less equal probability and amplitude from all directions, and the talker is relatively close and in front of the listener).
Use of a second-order directional microphone or array microphone having an AI-DI of 7 dB or more should bring some 60% of the subjects shown in Figure 3 to “0 dB normal” performance in typically diffuse background noise, and 80% within normal limits of ±3 dB around the average normal-hearing 0 dB SNR loss. Soede17-19 developed the Link-it™ array microphone that provides 8-10 dB improvement over a typical BTE omni microphone, and Siemens has recently introduced a practical version of a second-order microphone in its Triano hearing aid that delivers a similar improvement within a BTE aid. Considering that the difficulty of hearing in noise is the number-one complaint of hearing aid wearers, the development of second-order directional microphones is good news indeed. (Author’s Note: At the 1994 AAA convention, ER demonstrated a second-order ITE microphone27 with 7 dB AI-DI performance.)
Myth: All Directional Systems Provide Equal Benefit to Patients
We return to the fact that only 20% to 30% of the hearing aids dispensed feature directional microphones.3,5 This is perhaps not surprising since most dispensing professionals don’t assess the SNR handicap of their patients, and for the reasons discussed above, many of their patients report “directional microphones don’t work.” In addition, there is a mistaken belief by dispensing professionals that digital noise reduction can solve the problem by effectively increasing the wearer’s ability to understand speech in babble noise. Further obstacles in designing and evaluating directional hearing aids are illustrated in Figures 4-10.
.gif)
Venting and AI-DI. Figure 4 shows the effect of a typical vent combined with a directional microphone having an uncompensated low-frequency rolloff. Below about 900 Hz, the omnidirectional sound coming through the vent dominates, and the directional sound of the hearing aid is completely masked.
.gif)
Figure 5 from Burnett20 was an early documentation of this problem with venting. In this case, the high-frequency directivity was already small, so the estimated AI-DI drops from 1.2 dB to 0.2 dB with venting. This is an extreme example, but it illustrates that a large initial AI-DI is required of a hearing aid in order to maintain a good AI-DI after venting.
For open-ear, or nearly open-ear fittings, real-ear directivity at low frequencies can be preserved by introducing additional low-frequency gain, a design approach used by at least three manufacturers, including Etymotic Research.21-23
.gif)
Diffraction and the Testing and Measurement of Directivity. In Figure 6, hearing aids #1 and #2 showed better directivity when measured in a free-field (unmounted) than when measured on KEMAR. This illustrates the severe degradation in real-ear performance that can result from failing to take into account the diffraction around the ear.
.gif)
This design shortcoming continues in many present-day hearing aids, as indicated by the data on hundreds of hearing aids reported by Dittberner & Bentler24 and shown in Figure 7. Note that the average free-field (unmounted) ITE performance comes within 0.7 dB of the theoretically obtainable value, yet the average in-situ performance averages only 2.7 dB, 3.3 dB, and 3.5 dB AI-DI for the three types of ITE directional microphones.
.gif)
An industry average of 3.3 dB suggests that lesser designs range down to 2 dB and below. This was precisely what Christensen et al.25 found during measurements performed on 14 digital ITE directional hearing aids as shown in Figure 8. Two of the 14 aids had an AI-DI of approximately 2 dB. The data in Figure 8 represent the average of two directivity measures made on each hearing aid:
1) Polar directivity plots measured on the KEMAR manikin in Etymotic Research’s walk-in anechoic chamber, and
2) Diffuse-field directivity measured in Etymotic Research’s reverberation room. In the latter case, four matched loudspeakers driven from four non-coherent noise sources improved the room’s diffusivity, and the average of measurements made at several locations in the reverberation room provided a standard deviation of less than 0.3 dB at frequencies between 250 Hz and 6300 Hz.
Figure 9. Directivity data obtained at Etymotic Research on one C-MIC prototype mounted in mini- canal aid: 1. Three replications in walk-in anechoic chamber "free field." 2. Three replications in reverberation room "diffuse."
In checking the reliability and validity of these data, repeat measurements were made in both rooms on the same hearing aids. Figure 9 shows a set of such measurements made during the development of the SonionMicrotronic CC-Microphone.26 Both the test-retest and between-method agreement is good. We found that having both measurements available helped in the design of a complete directional-microphone or array-microphone.
Design Considerations and Microphone Matching. To return to the data shown in Figure 8, six of the first seven hearing aids (from the left) had been chosen as part of a quality-control check on the in-situ performance of microphones ER had either designed, helped design, or were designs of one of ER’s patent licensees. All of these aids had expected AI-DI performances of approximately 5 dB, and this expected performance held up through the complications of everyday manufacturing. When the seven ER-related hearing aids are excluded, nearly 30% (2 of the remaining 7 hearing aids) had AI-DI ratings of about 2 dB.
Despite the advantages sometimes claimed for dual-cartridge directional microphones, it is interesting to note that all but one of the lower-performance microphones tested were of the dual design; only one of the higher-performance microphones was. This is not surprising. Good directional performance in a single-cartridge directional microphone depends solely on making sure that the amplitude and phase response of the acoustic filters formed on the front and back of the diaphragm combine properly with the amplitude and phase response caused by diffraction around the ear. When tested on a manikin or human with the sound coming from the “null” angle, a nearly identical but opposite pressure in the front and back cavities is produced at each frequency. The microphone transducer itself does not enter into the directional performance; at the null angle, there is no pressure difference across the diaphragm, and so you could poke a hole in the diaphragm and not affect its directivity (such a hole would affect the sensitivity, of course). In practice, once the dimensions of the inlets and internal cavities of the microphone are locked into the metal forming tools, only the value of the easily controlled acoustical time-delay resistance affects the directional performance.
.gif)
For good directional performance with dual microphones, on the other hand, their sensitivity and response across frequency must be well matched in amplitude and phase. Figure 10 shows the effect of a slight mismatch in low-frequency cutoff on the directional performance of a dual-microphone directional with 5 mm physical spacing (approximately 4 mm effective acoustical spacing). At low frequencies, the microphone effectively points backwards!
In addition to the problem of obtaining matched microphones in the first place, the high-sensitivity, low-noise electret microphones now used in hearing aids sometimes change in sensitivity and frequency response after temperature and humidity cycling, and the clogging of ports with debris.28,29 Thus, even when two microphones start out well matched, subsequent differential changes can reduce the AI-DI. Whatever the explanation, the measured results suggest that the “dual is better” principle is not supported in the real world or in the hearing instrument literature.30
“I Hear Better Without My Hearing Aids”
The above statement can be readily understood in the case of hearing aids with low directivity and typical digital bandwidth. First, in typical cocktail-party noise levels of 82-85 dB SPL (ie, 70 dB HL), the background babble would mask all but the most intense 10 dB of the dynamic range of the desired talker’s speech cues. Thus, someone with less than a 60 dB audiometric loss would hear all the available speech cues unaided.
.gif)
Second, as shown in Figure 8, a significant number of directional-microphone digital hearing aids have an AI-DI of 2 dB in a hearing aid with limited bandwidth. The average bandwidth we measured on the digital aids shown in Figure 11 was only 5.8 kHz. AI calculations (SII) for a hearing-impaired subject with 8 dB SNR loss indicate that a 0.9 dB higher SNR is required when the bandwidth is limited to 5.8 kHz (see Killion & Christensen31). As a check, we filtered alternate QuickSIN test lists (female talker) with a 5.8 kHz low-pass filter and tested 14 hearing aid wearers as open-ear subjects at 70 dB HL presentation level. The average SNR required by 13 of the subjects was 1.0 dB higher in the filtered condition (the standard error of the mean difference for two lists/condition was 0.4 dB). The 14th subject—who may have substantial inner hair cell loss at low frequencies—required 7.5 dB greater SNR when the frequencies above 5.8 kHz were eliminated. The combined effect on speech understanding of a 2 dB AI-DI and a 5.8 kHz bandwidth is that such a hearing aid has an effective advantage in SNR over the amplified open ear of only 1 dB (ie, 2 dB minus 1 dB because of the limited bandwidth).
Third, additional distortion introduced by noise reduction, feedback reduction circuits, and response irregularities can take a further toll. This is shown in Figure 11, which plots the SNR required for 50% correct responses for words in sentences with the digital hearing aids reported on in Part 11 of this three-part series of articles.
The only explanation for the data in Figure 9 is that the signal processing of these hearing aids was not helping under high noise-level conditions when the speech peaks were only 10-15 dB above the noise. Indeed, the author has had just that experience recently with two different models of recently purchased digital hearing aids. Switching to directional mode almost made up for the deficiencies in the hearing aids. Unless the directional microphones were activated, I could hear much better with my own ears in a noisy restaurant.
.gif)
Directional Microphones in Reverberation
Figure 12 illustrates a case in which the directional microphone provides no benefit. The distinguishing feature is the same one reported most recently by Walden et al.6 and Rickets12: the distance to the talker exceeds the critical distance.
In Figure 12, the “noise” is the previous speech sounds of the talker, which hang on as if they are maskers. The signal-to-noise ratio is thus determined by the ratio of direct (speech) versus reverberant sound (echo). When listeners sit in the rear pew of a church, they are located well beyond the critical distance, so the reduction in reverberation provided by a directional microphone may leave the reverberation still dominant.
To prevent disappointment with directional microphones, the dispenser can do two things:
1) Select directional hearing aids with real-world AI-DI of 5 dB or better, and
2) Counsel the patient that the directional microphones can be expected to provide significant benefit when the talker is relatively close and in front of them, and the noise arrives mostly from the sides and the back. However, relatively little benefit may be realized when the talker is at a distance or behind the hearing aid user and/or the majority of the noise arrives from in front.6,12,35
With those two caveats in place, the author’s experience is that directional microphones and array microphones can make a reliable, significant—and sometimes dramatic—difference in the ease of understanding in noise. Kochkin32 reported a 90% satisfaction rate for a BTE directional aid with a directional-vs-omni difference of 5 dB. And the hearing industry continues to make progress: On a sample size of 757 directional hearing aids, Kochkin33 reported overall customer satisfaction of 81%, which equalled the US customer satisfaction rating for all consumer electronic products, and exceeded the satisfaction rating for the best computers!
All signs point to the conclusion that there should be a good directional microphone in every hearing aid.

|
References
1. Killion MC. Myths that discourage improvements in hearing aid design. Hearing Review. 2004;13(1): 20-24.
2. Kochkin S. The VA and direct mail sales spark growth in hearing aid market. Hearing Review. 2001;8(12):16-24,63-65.
3. Kochkin S. 10-year customer satisfaction trends in the US hearing instrument market. Hearing Review. 2002; 9(10):14-25,46.
4. Kochkin S. Consumers rate improvements sought in hearing instruments. Hearing Review. 2002; 9(11):18-22.
5. Strom KE. The HR 2003 dispenser survey. Hearing Review. 2003;10(6):22-38.
6. Walden BE, Surr RK, Cord MT. Real-world performance of directional microphone hearing aids. Hear Jour. 2003; 56(11):40-47.
7. Cox RM, Alexander GC, Gilmore C, Pusakulich KM. Use of the Connected Speech Test (CST) with hearing-impaired listeners. Ear Hear. 1988;9(4):198-207.
8. Julstrom S. A new approach to automatic mixing. J Audio Eng Soc. 1984; 32(7-8): 490-495.
9. Niquette P, Gudmundsen G, Killion M. QuickSIN Speech-in-Noise Test Version 1.3. Elk Grove Village, IL: Etymotic Research; 2001.
10. Valente M, Fabry DA, Potts LG. Recognition of speech in noise with hearing aids using dual microphones. J Am Acad Audiol. 1995; 6:440-449.
11. Preves DA, Sammeth CA, Wynne MK. Field trial evaluations of a switched directional/omnidirectional in-the-ear hearing instrument. J Am Acad Audiol. 1999; 10:273-284.
12. Ricketts T, Henry P, Gnewikow D. Full time directional versus user selectable microphone modes in hearing aids. Ear Hear. 2003;24:424-439.
13. Cox RM, Gilmore C, Alexander GC. Comparison of two questionnaires for patient-assessed hearing aid benefit. J Am Acad Audiol. 1991; 2:134-145.
14. Mueller G. Fitting test protocols are “more honored in the breach than the observance.” Hear Jour. 2003; 56:(10): 19-26.
15. Cannito L, Taylor B. The relationship between SNR loss and the audiogram. Poster presentation at: American Academy of Audiology Convention; Apr 4, 2003; San Antonio, Tex.
16. Arcaroli J. Cochlear America’s data on 19 recent cochlear implant patients. Englewood, Colo: Cochlear America; 2001.
17. Soede W. Improvement of speech intelligibility in noise [PhD dissertation]. Delft University of Technology, The Netherlands; 1990.
18. Soede et al. The Array Mic [brochure]. Elk Grove Village, IL: Etymotic Research; 2000.
19. Christensen LA, Helmink D, Soede W, Killion MC. Complaints about hearing in noise: A new answer. Hearing Review. 2002; 9(6):34-36.
20. Burnett E. Effect of large vent on directivity of BTE hearing aid. Seminar presented at: ANSI Standards Meeting, 1990.
21. Flynn MC. Opening ears: The scientific basis for an open ear acoustic system. Hearing Review. 2003; 10(5):34-37.
22. Killion MC, Wilson DL. Response-modifying earhooks for special fitting problems. Audecibel. 1985; 34(4):28-30.
23. Groth J, Pedersen BD. A high-definition compression system for open fittings. Hearing Review. 2003; 10(4):68-69,81.
24. Dittberner A, Benter R. Interpreting the Directivity Index (DI). Hearing Review. 2003; 10(6):16-19.
25. Christensen L, Schulein R, Monroe T, Haapapuro A, Killion MC. Performance measures on ITE directional hearing aids. Seminar presented at: American Academy of Audiology Convention, May 2001; San Diego.
26. SonionMicrotronics. Technical data sheet for Microphone Unit 6950 (v. 1.2). Minnetonka, Minn: SonionMicrotronics; 2000.
27. Killion MC, Waldhauer F, Wittkowski J, Goode R, Allen J [inventors]. Hearing Aid Having Plural Microphones and a Microphone Switching System. U.S. Patent No. 5,524,056; 1996 (filed Apr. 12, 1994).
28. Kuk F, Baekgaard L, Ludvigsen C. Design considerations in directional microphones. Hearing Review. 2000; 7(9):68-73.
29. Tchorz J. Effects of microphone matching in directional hearing instruments. Hearing Review. 2001; 8(10):54-58.
30. Thompson SC. Dual microphones or directional-plus-omni: Which is best? In: Kochkin S, Strom KE, eds. High Performance Hearing Solutions, Vol 3. Hearing Review. 1999; [suppl] 6(1):31-35.
31. Killion MC, Christensen L. The case of the missing dots: AI and SNR loss, Hear Jour. 1998; 51(5): 32-47.
32. Kochkin S. Customer satisfaction and subjective benefit with high performance hearing aids. Hearing Review. 1996; 3(12):16-26.
33. Kochkin S. On the issue of value: Hearing aid benefit, price, satisfaction, and brand repurchase rates. Hearing Review. 2003; 10(2): 12-26.
34. Revit LJ, Schulein RB, Julstrom SD. Toward accurate assessment of real-world hearing aid benefit. Hearing Review. 2002;9(8):34-38,51.
35. Surr RK, Walden BE, Cord MT, Olseon L. Influence of environmental factors on hearing and microphone preference. J Am Acad Audiol. 2002; 13:308-322.
Correspondence can be addressed to HR or Mead C. Killion, PhD, Etymotic Research, Elk Grove Village, IL 60007; email: [email protected].

.gif)
.gif)
.gif)
.gif)