When dispensing professionals face the problem of occlusion, they are offered a variety of choices—some of which are contradictory. Sometimes increasing the low frequency gain helps; sometimes decreasing the low frequency gain helps. Frequently, shortening the length of the vent or enlarging the width of the vent helps. Sometimes increasing the SSPL 90 helps; sometimes increasing the TK helps. This article proposes that the HAO effect is a distinctly different phenomenon from the threshold occlusion effect for at least four reasons.
Everyone who has fit hearing aids has had to deal with the “occlusion effect” which is often described by patients as a hollow or echoing sound when speaking. For the dispensing professional, it can be difficult to solve this problem, and most experienced clinicians employ a variety of approaches to reduce or eliminate occlusion—many of which often seem contradictory.
This article will look at the hearing aid occlusion effect (HAO) as a distinctly different entity compared to the occlusion effect as it relates to bone conduction threshold measures. There are four reasons why the HAO is perceptually different from threshold occlusion measures:
1) HAO is the result of self-generated sounds, while threshold occlusion is an externally generated sound;
2) Sound transmission through the skull is faster than sound transmission through the air;
3) Hearing aid processing delays accentuate the bone vs air variances, thereby increasing the perception of an echo from one’s voice;
4) Acoustic signals from a hearing aid interact with the self-generated acoustic signals.
HAO is Self-Generated
The conventional definition of the occlusion effect is a resulting increase in the bone conduction thresholds for frequencies below 1 kHz when the ear is covered with an earphone. This effect has been attributed to the out-of-phase vibration of the mandible relative to the vibration of the skull for low-frequency sounds. While this may be helpful in understanding threshold measurements, it does not adequately explain the occlusion effect induced by a hearing aid.
It may be helpful to view these effects as different phenomena. In fact, there is a significant difference: during bone conduction testing, the signal is an externally generated sound (ie, bone conduction vibrator) while the HAO is usually an internally generated signal (ie, the patient’s own voice or internal chewing noise). Patients with HAO rarely complain that their “bone conduction thresholds are lower,” but they do often complain that their own voice sounds louder, has an echo, or is hollow sounding.1 With this in mind, many of the traditional assumptions regarding the occlusion effect as it relates to the bone-conduction testing may not hold true for the HAO patient.
Killion, Wilbur & Gudmundsen2 reported that vowel sounds which measured 70 dB SPL at the mouth can result in up to 140 dB SPL in the occluded ear canal. As sound passes through the skull from the oral cavity, it is magnified supposedly by the out-of-phase vibration of the mandible against the cartilaginous ear canal.3 When the ear canal is occluded with a hearing aid, the natural outflow of this sound is impeded by the aid, thereby inducing the increased sound pressure. This out-of-phase vibration generates a sound which is normally vented from the ear when the ear is unoccluded, but is trapped in the ear canal when the canal is occluded by a hearing aid. This same rationale was used by Bekesy4 to explain why bone conduction thresholds are lower when the ear canal is occluded with an earphone and are greatest for frequencies below 1000 Hz. However, if the mandible is creating an out-of-phase signal, why isn’t the primary signal made less intense or canceled altogether?
Additionally, many custom hearing aids, particularly CICs, extend medially into the bony portion of the ear canal, but the patient still reports symptoms which are often attributed to occlusion. If the adult human ear is approximately 2.5 cm in length5 and the cartilaginous section constitutes the outer 0.8 cm to 1 cm, then any hearing aid that extends into the ear canal 1 cm or beyond may be eliminating the cartilaginous vibration from the mandibular action, and the source of the HAO must be coming from somewhere other than the mandible.
So what generates the symptoms we refer to as HAO? This is most likely the result of self-generated intra-oral sounds that set the bony portion of the ear canal, the middle ear, and the cochlea into vibration. Such vibrations can increase the sound pressure generated in the ear canal and are trapped there by the presence of a hearing aid.
Work at Ohio University by the author measured the shift in bone conduction thresholds with TDH 49 earphones and MX41/AR biscuit-type cushions, as well as with EAR plugs occluding the ears. The data suggest that the occlusion effect results in different degrees of threshold shift when the ear canal is occluded with a sound-attenuating plug than when the canal is occluded with an earphone. This is to be expected since the earphone does not create a tight seal around the ear and also has a much larger volume of air trapped between the earphone cushion and the eardrum than a sound-attenuating plug.6 In addition, test subjects were asked if their words sounded different with the earphones or the plugs inserted. Regardless of the mechanism of occlusion (earphone vs earplug), not all subjects reported a change in their own voice in spite of a bone conduction threshold shift. In fact, some subjects reported no change in the perception of their voice (ie, no HAO)!
Is it often suggested that there is no occlusion effect if there is low frequency hearing loss, yet Naughton6 clearly showed a bone conduction occlusion effect at 500 Hz with hearing loss up to 60 dB. In clinical practice, the author regularly encounters patients with low frequency hearing loss who complain of HAO.
Sound Transmission is Faster in a Solid
Another component of the HAO is due to the difference in the velocity of sound in bone vs air. Sound travels faster in a more dense medium (bone) than it does in a less dense medium (air).7 Sound generated in the oral cavity and emitted from the mouth takes a few milliseconds longer to reach the ear canal than sound passing through the bones of the skull. In research on stuttering, the sound emitted from the mouth that travels to the ear is called “side tone.” Changes in side tone can alter the perception of the strutterer’s own voice and decrease stuttering behavior. This delay could conceivably be one of the reasons for the resulting echo of HAO. Additionally, the length of the signal pathways are different for oral signals than for internally generated bone conduction signals. Specifically, sounds emanating from the mouth must travel approximately 12 cm-15 cm before reaching the ear, while sounds produced in the oral cavity traveling through bone travel only 1 cm-2 cm. As a result, the intra-cranial signal arrives in the external canal much faster.
Hearing Aid Processing Times
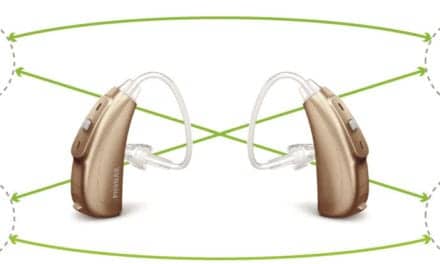
With HAO, an air-conducted sound emitted from the mouth is further delayed by a few milliseconds by the inherent time required for the sound to be processed by the hearing aid, particularly with digital hearing instruments. While this component of HAO is present with both analog and digital instruments, the complexity of digital signal processing (DSP) may have added additional processing time, as well as phase differences. Frye8 has reported that the time required for a sound to be processed in a DSP aid is longer than for an analog aid. As a result, patients who attempt to wear a digital aid in one ear and an analog aid in the other (or, potentially, two digital aids with significantly different processing times) may not like the sound system, as the signal arrives in the cochlea slightly delayed in one ear relative to the other. This delay adds to the time differential created by the velocity variances of bone vs air, thereby enhancing the echo effect. Van Vliet9 reported a study which indicated that, with DSP hearing aids, a 3-5 msec processing delay is noticeable 75% of the time, and a delay of more than 10 msec is objectionable 90% of the time. Interestingly, he reported HAO-like problems with digital aids that were apparently resolved with a change to analog aids.
Hearing Aid and Ear Interactions
It may be helpful to consider the HAO as an active dynamic process involving the ear canal, middle ear, and inner ear, with the sound generated by the hearing aid. To explore this process, it is helpful to review some of the literature on the generation of bone-conducted sounds.
Naunton6 reported that there are two types of bone conduction: inertial and compressional. Intertial bone conduction results from the fact that, at low frequencies, the ossicles and the mandible move out of phase with the rest of the skull, thereby transmitting a signal to the cochlea. As the ossicles sway in the middle ear, they induce a signal that is out of phase with the signal generated by the bony portion of the ear canal and the walls of the middle ear. This out-of-phase sway results in a direct stimulation of cochlear fluids. Simultaneously, the mandible moves out of phase with the rest of the skull, further adding to the intra-cranial-generated signal.
Compressional bone conduction, in contrast, occurs when the skull vibrates sufficiently to induce compression of cochlear fluids. Depending upon the frequency, the skull may be moving in an anterior-posterior or a lateral-medial direction as it goes through the compression/rarefaction cycles.
Inertial bone conduction responds to lower frequency signals, while compressional bone conduction responds to higher frequency signals. However, both types of bone conduction may be operational at all frequencies. The production of 140 dB SPL in the ear canal—as reported by Killion, Wilbur & Gudmundsen2—from vowel sounds should be more than adequate to induce both inertial and compressional bone conduction.
Allen & Fernandez10 suggested that sound generation in the external meatus has little importance, and attributed the occlusion effect to an increase of middle ear impedance and the subsequent transmission loss of energy to the inner ear from the conductive mechanism of the ossicular chain. They attributed the lack of occlusion present when the external canal is occluded in the bony portion of the canal to the substantial transmission loss. They also suggested that middle ear lesions influence the vibratory mechanism of the inner ear so as to produce intensity and phase distortions. Such intensity and phase distortions presumably may also be present with the hearing aid fitting, as the hearing aids may be out of phase with each other8 or with the reflected sound from the eardrum, thereby contributing to the HAO.
The ossicles also conduct energy from the cochlea back to the ear canal, as documented with otoacoustic emissions (OAE). The detection of the OAEs is reduced with changes in the pressure of the outer ear canal.11 Accordingly, the “backward flow” of energy from the cochlea may be expected to interact with the “forward” flow of energy from the hearing instrument.
Additionally, the placement of a hearing aid into the ear canal creates a Helmholtz resonator: the air bolus between the tip of the hearing aid and the eardrum constitute a major cavity, and the vent constitutes the resonator.12 The middle ear impedance also affects this resonator. The medial end of the resonator (ie, the eardrum) is usually not a hard wall (except in cases involving tympanosclerosis, etc), but rather a dynamic entity controlled by the cochlea, middle ear muscles, and the Eustachian tube.
Huizing13 suggested that the peripheral auditory system should be viewed as a complex vibratory unit whereby changes in mechanical impedance at one point influence the entire mechanical system. This concept was advanced further by Allen & Fernandez10 who indicated that impedance variations in the external and middle ear may lead to impedance changes in the inner ear fluids. Additionally, Lybarger14 reported that the impedance of the eardrum can affect the performance of the earphone-earmold-ear response.
Accordingly, occlusion of the external auditory canal may result in an impedance mismatch between the inner ear and the conducting system, thereby reducing energy transfer. Feldman & Wilbur15 reported that “the most effective energy transfer occurs when a force flows from one medium to another of a like impedance” (p.2). The middle ear mechanism serves as an impedance matching transformer to overcome the difference in the impedance of air and the impedance of cochlear fluids. This transformer, however, may add an additional source of impedance: it should be remembered that this is a dynamic air-filled cavity, as the Eustachian tube is intermittently changing the middle ear pressure and the impedance at the eardrum. When the pressure of the air is the same on both sides of the eardrum, energy transfer is maximized; conversely, when the ear pressure on each side of the eardrum is different, there is reduced transfer of energy as more sound is reflected from the eardrum. This may result in an increased potential for HAO or even acoustical feedback.
The concept of impedance is one way to describe the ability to transfer energy from one medium to another. It is the complex interaction of the resistance and the reactance of the ear. Resistance is the component of impedance that results in a dissipation of energy from friction. It is essentially frequency-neutral, affecting all frequencies the same; however, the reactances have a differential frequency effect. Reactance refers to the system’s ability to store and return energy to the source. There are two types of reactances: capacitive and inductive. The stiffness or capacitive reactance is inversely proportional to frequency, and is greater at the lower frequencies. Conversely, mass reactance is directly proportional to frequency, and is essentially negligible at lower frequencies. So, as the mass increases, the net effect is to decrease the higher frequencies. Because these reactances are vectors, they are interactive such that one cannot change one without affecting the other. The frequency region where the stiffness and mass reactances are balanced is the resonant frequency of the system.7.15 This point is important as many authors discuss the various resonant peaks and ignore the fact that the resonant peaks are the direct result of the reactances. Any acoustical changes that affect the resonant peaks are actually changes in one or both types of reactances.
It is reasonable to assume that the impedance of the ear canal interacts with the impedance of the hearing aid.12,14 This effect is most commonly seen as a change in the acoustical resonance of the ear canal. While the resonance of the normal adult unoccluded ear canal is in the frequency region of 2800 Hz-3300 Hz, the occluded ear canal resonance tends to be higher due to the smaller cavity volume formed between the receiver and the eardrum, resulting in a change in the acoustical reactances. Speaks7 stated that “the natural frequency of a system is directly proportional to the square root of its stiffness and inversely proportional to the square root of its mass” (p.81). Since a smaller cavity volume can be expected to have greater stiffness,12 the natural frequency (ie, resonant frequency) will increase. This may contribute to the assertion that increasing the depth of insertion of a CIC hearing aid may increase the high frequencies, as well as decrease the perception of HAO.
The phase of the signal from the hearing aid will also interact with the intra-cranial signal to effect energy flow. Van Kamp & Wouter16 stated:
“…there is an average power transfer to a system if the force-like quantity (velocity, pressure, voltage, etc) is in phase with the velocity-like quantity (velocity, volume velocity, electrical current). If these quantities are in quadrature, which means that the phase difference equals +90 degrees or –90 degrees, no average power transfer takes place.” (p.313)16
What this means for a hearing aid fitting is that the signal being delivered to the ear canal must be in phase with the signal created in the ear canal (from all of its various sources). If not, there is poor energy transfer (ie, the patient does not hear well or complains of HAO). Another way of stating this is that there is an impedance mismatch between the hearing aid and the ear.
Van Kamp & Wouter16 also stated that “the amplitude is not sufficient to characterize the force completely, because the phase information is still lacking” (p.135).16 This suggests that, because of the differences in phase between the hearing aid and the intra-cranial signal, the sound from the hearing aid may interact with the sound of the ear canal, distorting the signal perceived by the patient. These researchers point out that the sound pressure in the ear canal should be seen as the result of the input sound pressure (eg, from the hearing aid) and the pressure reflected from the eardrum. I would add that an additional source of pressure is the sound generated by the walls of the ear canal and the middle ear space.
Conclusion
When dispensing professionals face the problem of occlusion, they are offered a variety of choices—some of which are contradictory. Sometimes increasing the low frequency gain helps; sometimes decreasing the low frequency gain helps. Frequently, shortening the length or enlarging the width of the vent helps. Sometimes increasing the SSPL 90 helps; sometimes increasing the TK helps. The variety and contradictory nature of these solutions to the HAO problem are “hit or miss” or derived from “clinical intuition.” This article proposes that the HAO effect is a distinctly different phenomena from the threshold occlusion effect for at least four reasons. A re-thinking of the process may be in order to develop more effective solutions to help solve patients’ HAO complaints.
| Richard Navarro, PhD, is an audiologist at Active Hearing and Balance Center Inc, Houston, Tex. |
Correspondence can be attributed to Richard Navarro, PhD, 2622 Fondrel, Houston, TX 77063; email: [email protected].
References
1. Pogash R, Williams C. Occlusion and own-voice issues: Protocols and strategies. Hearing Review. 2001; 8(3): 48-54.
2. Killion M, Wilbur L, Gudmundsen G. Zwislocki was right…a potential solution to the "hollow voice" problem. Hear Instrum. 1986; 39: 14-17.
3. Zwislocki J. Cited by: Naunton RF. The measurement of hearing by bone conduction. In: Jerger J, ed. Modern Developments in Audiology, New York: Academic Press; 1963.
4. Von Bekesy G. Experiments in Hearing. New York: McGraw Hill; 1951.
5. Wilbur L. Anatomy and physiology of the middle ear. In: Feldman AS, Wilbur LA, eds. Acoustic Impedance and Admittance: The Measurement of Middle Ear Function. Baltimore: William and Wilkens; 1976.
6. Naunton R. The measurement of hearing by bone conduction. In: Jerger J. ed. Modern Developments in Audiology. New York: Academic Press; 1963.
7. Speaks C. Introduction to Sound: Acoustics for the Hearing and Speech Sciences. San Diego: Singular Publishing Group Inc; 1992.
8. Frye G. Testing digital and analog hearing instruments: Processing time delays and phase measurements. Hearing Review. 2001: 8(10): 34-40.
9. Van Vliet D. It was a dark and stormy night. Hear Jour. 2002; 55:72.
10. Allen G, Fernandez C. Cited by: Naunton RF. The measurement of hearing by bone conduction. In: Jerger J, ed. Modern Developments in Audiology. New York: Academic Press; 1963.
11. Navarro R, Frasier J, Clark A, LeBlanc E, Christiansen L. Distortion product otoacoustic emissions under varied ear canal pressures (poster session). Presented at: ASHA Convention; Nov 17, 2000; Washington, DC.
12. Cox R. Acoustical aspects of hearing aid-ear canal coupler systems. Monographs in Contemporary Audiology. Minneapolis: Maico Hearing Instruments; 1979.
13. Huizing E. Cited by: Naunton RF. The measurement of hearing by bone conduction. In: Jerger J, ed. Modern Developments in Audiology. New York: Academic Press; 1963.
14. Lybarger S. Earmolds. In: Katz J, ed. Handbook of Clinical Audiology. Baltimore: Williams and Wilkens; 1978.
15. Feldman A. Wilbur l (eds). Introduction. In: Acoustic Impedance and Admittance: The Measurement of Middle Ear Function. Baltimore. William and Wilkens; 1976.
16. Van Kamp K, Wouter C. Principles of acoustic impedance and admittance. In: Feldman AS, Wilbur LA, eds. Acoustic Impedance and Admittance: The Measurement of Middle Ear Function. Baltimore. William and Wilkens; 1976.