Custom fittings require an understanding of the residual auditory area
This article is designed to reinforce and simplify what, in another earlier article, we have called a “paradigm shift” brought on by advanced technology and an increased understanding of the auditory system. We have addressed the methods by which we can transition our practices from “what we were taught” into “what we need to know, and do now.” This is not about a new way of doing things; it is about a new way of thinking about things.


|
| Jay B. McSpaden, PhD, BC-HIS, is an audiologist who retired from private practice and currently practices as a hearing instrument specialist in Jefferson, Ore. Larry Brethower, ScD, BC-HIS, is a hearing instrument specialist who has been licensed in Missouri for 24 years, with 9 years of consulting/dispensing in Oregon. |
Let’s address the subject of music. It doesn’t matter what kind. We can talk about the glory of the Three Tenors, or Il Divo, or Josh Grodin; or about the benediction that is a Faith Hill or a Whitney Houston singing gospel; it’s about the amazing purity and pitch of Celine Dionne and Barbra Streisand, and about the fun of the Manhattan Transfer, or the Nylons. It’s about Loreena McKinnock singing Irish ballads, and Joan Baez singing Villa-Lobos. It’s about the sultry, torch of a Nina Simone, and the husky smoke of Carly Simon. It’s about the taps of a Gregory Hines, the toe-shoe whisper of Baryshnikov, and even the percussion that is River Dance. It is about the strengths of Garth Brooks and Trisha Yearwood, and the gravel and grit of the Boss or Judy Henske. And, it’s about orchestral music, and solo instruments, as well. It’s, about The Mormon Tabernacle Choir and Gregorian chant, and even the Carmina Burana. It’s also about talking books and audio books that contain the musical prosody that is poetry.
Music is one facet of the diamond that is sound. Music is, to our brain and soul, what spice is to our food. It gives it zest, and flavor and panache. For most people, it is far more important than simply being able to hear the news or baseball on the radio at 40 dB. And, as the marvelous Don Harris, PhD, once asked in a 1971 closing lecture at the AAS Seminar on Hearing Aids and Profound Sensori-Neural Hearing Loss, “…which demands more of a hearing aid?”
Virtually anyone can “first-fit” a hearing instrument—yielding what, in many cases, resembles a digitized, analog fitting. Hearing instrument manufacturers will tell you that a large percentage of the units returned for credit have never been adjusted from their initial “first-fit” settings. It’s difficult to believe there is no correlation here; we need to utilize fully the available technology to produce satisfied patients.
We Don’t Hear with Our Ears; We Hear with Our Brains
Hearing aids do not change hearing; hearing aids change the sound that people hear. They change sound in such a way that, whatever hearing a patient/client has retained, they can use it more efficient. If a hearing aid doesn’t make you communicate more effectively, it is not worth having. If a hearing aid does help you communicate more effectively, there is high probability that you will think it’s worth having. Kochkin has demonstrated fairly convincingly that “benefit clearly overwhelms price as the key determinant of customer satisfaction, and technology does make a difference.”1
For example, a CROS hearing aid does not improve the hearing in either ear. It does not improve the hearing in the “bad” side, where the microphone is located, and it doesn’t improve the hearing in the “good” side, because that was the good side. But, it makes people communicatively more efficient, in which case, it’s worth having.
Value, communication and utility. One problem we have in the dispensing profession is the perception of received value on the part of our patients. We do not point out to them that the value they receive from the hearing instrument is the improvement in communication efficiency. Because, in many cases, we have not provided for them with the appropriate criterion for judgment, they cannot evaluate whether it helps them communicate better. When we do give them that information, we provide for them what “realistic expectations” for the instrument should be.
Manufacturers are now building hearing aids that amplify at 3000-6000 Hz, and even more. If they’re going to build hearing aids that amplify to 6000 Hz, shouldn’t dispensing professionals know what the ear does at 6000 Hz? Manufacturers are trying to approximate with their hearing instrument technology what Christopher Schweitzer, PhD, has called “bio-mimicry.”

|
| FIGURE 1. The patient’s residual auditory area or dynamic range—the area where speech energy can be placed for maximum effectiveness—is defined by the speech reception threshold (SRT) and the uncomfortable loudness level (UCL). |
Addressing loudness growth. Patients will not wear anything that hurts them. This shouldn’t surprise us. Why would they wear a hearing aid that hurts? Why would they wear a hearing aid that is so loud, or so raspy, or so “out of control” that they have to turn it down in a wide variety of important listening situations in order to tolerate it? If they turn it down until it’s no longer effective in noise (ie, turning it into an earplug), it isn’t worth what they paid for it—no matter what the price was. Similarly, if they purchased a hearing aid to hear better in a specific listening situation, then cannot use the aid in that situation, they will express dissatisfaction (although not necessarily to you).
Dispensing professionals need to know “how loud” is “too loud”. Discomfort with loud sounds is still a major source of problems hearing aid users, with 28% of wearers expressing at least some dissatisfaction in this area.2 This simply shouldn’t be the case with our modern testing/verification equipment and advanced hearing instruments. We know where the threshold is. Where’s the MCL or UCL? Each of us exhibits loudness growth differently at each frequency in each ear. Recruitment, which is part of this process, is caused by an internal change in the hair cells, and the loss of the outer hair cells is what starts it. Loudness is a process of changes in perception.
Recruitment starts at threshold. You can fit hearing aids to patient’s ears until your hands fall off, and you will satisfy patients only partially (and, only part of the time) without accounting for their recruitment. However, if you fit every hearing aid by binaurally balancing the signal—at MCL—in the center of the patient’s brain, you will rarely have a dissatisfied customer.
The author’s personal preference in this portion of the dispensing/fitting process is to test with pure-tones, test speech using the live voice of the patient’s partner and/or real-world stimuli, establish MCL with that same voice, map out the perimeter of the residual auditory area, establish the UCLs at frequencies with tones and/or reflexes, and fully stimulate their residual ability.

|
| FIGURE 2. The black bars show the dynamics of an amplified average conversational speech signal. If there was no compression for speech in this aid, then the length of all the bars would be about 30 dB. Since there is compression, some bars are considerably shorter than 30 dB, effectively placing the sound in the patient’s residual auditory area. |
This process takes a little longer, but like anything else, it isn’t practice that makes perfect; it’s perfect practice that makes perfect! We take the somewhat unorthodox stance that it is still important to take pure-tone threshold measurements, because without those measurements it’s difficult to understand what the effect of MCL and UCL is going to be. Note that we don’t think pure-tone thresholds per se are vital; the idea is that dynamic range represents a range between the speech reception threshold (SRT) and the threshold of discomfort (UCL). If there is a hearing loss, what you essentially have is a “loudness pad,” because you’re carving things off the “bottom” of the audiogram, but you’re not really taking anything off the top.
Discomfort occurs at roughly the same threshold for each ear. The ear goes “nonlinear” at about the same spot whether there’s a “loudness problem” in it or not. You are still putting the same amplitude wave in that cochlea. At this point, we tell the patient: “I want you to adjust this tone [a 40 dB tone at 2000 Hz] until it sounds equally as loud as a 1000 Hz sound at 40 dB.” If at 500 Hz, the signal sounds as loud as it did at 1000 Hz; and at 250 Hz it sounds as loud as it did at 1000 Hz; and at 125 Hz it sounds as loud as it did at 1000 Hz, 2000 Hz, 3000 Hz (and 4000-8000 Hz), etc, then you’ve created an Equal Loudness Curve. Because the patient’s judgment at every one of those points is equal to a 40 dB loud signal at 1000 Hz, we arrive at a family of curves that may have less distance between equal-loudness increments.
How do we use these? Equal loudness curves can be confusing. The reason is because we usually see an audiogram that has flat parallel lines. However, what the patient’s brain perceives is not as simple as what is displayed on the audiometer. Equal loudness curves are important for patient comfort and auditory perceptual differences. The frequency response at 6000 Hz has an awful lot of information. In fact, all of a sudden, what happens to loudness growth at 2000 Hz, 3000 Hz, 4000 Hz, and 6000 Hz matters! Patients have recruitment problems at the frequencies where they have hearing loss. When they recruit, this MCL-UCL difference looks to only be 2, 6, 7, 8 dB. However, if loudness is growing at a ratio of 3:1, every time you turn up sound level by 1 dB on the dial, the patient perceives a 3 dB difference. If you turn it up 10 dB, the brain perceives a 30 dB difference. It’s important to know how loud it is to the patient at 2000 Hz, at 3000 Hz, 4000 Hz, and 6000 Hz. It tells us how much compression we have to initiate on the aided signal.

|
| FIGURE 3. Speech sounds below the threshold (dB PL) as a function of frequency will not be audible. For example, average conversational speech above 750 Hz is inaudible for this individual. |
Much of our equal loudness data (in phons) comes from Fletcher & Munson.3 These researchers generated this information in 1933—6 years before the lead author of this paper was born! So, this isn’t any new breaking research; we’ve just never known how to use it properly.
Few of us spend time talking about the concept of pitch and high-frequency hearing (ie, the mel scales). If we raise the intensity of the sound at 4000 Hz or higher, the signals go up in pitch perception. When we introduce a sound with a high frequency and we get a high intensity at that high frequency, we shift the perception of pitch upward. Is it possible that modern hearing aids, which have begun to amplify at 3000-6000 Hz, may be putting too much amplification in those frequencies, thereby driving the perceived pitch upward? If this is done, it can distort the perception of the speech information. It is shifted beyond the point where the patient can easily or correctly perceive it. At that point discrimination goes down instead of up. By over-fitting, we may not improve communication or discrimination; instead we may make it worse! And this brings us back to why it’s important to know what’s occurring at the higher frequencies.

|
| FIGURE 4. Correction of hearing loss based on a current gain fitting formula with a current WDRC hearing aid. |
Most readers of this magazine have knowledge of phonemes and phoneme charts, including those at 4000 Hz, 5000 Hz, and 6000 Hz. Most of your patients are going to have the hearing loss up in the high frequency region. If we make these high frequency sounds too loud, we may actually be altering their ability to detect phonemes. But now, it is not the same mixture of perceptions that comprise “normal speech,” rather it’s distorted. The patient’s ear can now detect the /h/ or /ch/ or /sh/ or /f/. However, because it is shifted upward (because we made it louder at the higher frequencies) it’s no longer /h/ or /ch/ or /sh/ or /f/ that the patient perceives.
Traditionally, we over-fit hearing aids for the high frequencies because we didn’t understand the UCL/MCL relationships. Our thinking has been “we’ve got to have more power” without thinking “we’ve got to have more control” relative to the higher frequencies. As the patient’s dynamic range gets narrower, we ML need enhanced control.

|
Goal: Adjust the parameters on the hearing aid to ensure: 1) Audibility and comfort for an amplified average conversational speech signal. 2) Audibility and comfort for other types of speech signals (soft and loud speech) 3) That loud sounds are not uncomfortably loud across all frequencies. 4) Audibility across the broadest frequency range possible. |
| FIGURE 5. The goal of complete stimulation of a patient’s residual auditory area. | |
Back to Basics
The history of hearing aid fitting has been limited by the concept that all we really needed to do is replace intensity at frequencies damaged or destroyed by pathology in each ear. It is clear that if all it would take was replacing that energy at those frequencies in order for a person to return to “normal” hearing, we would have been able to make perfect fittings at any time for the past 40 years.
Although it is not that simple, today the perfect fitting is more attainable. There have been many fitting formulae theorized and researched in an attempt to “correct” an identified hearing loss. The idea of a “target” is a starting point—not a prescriptive requirement. The target represents what would be the best frequency and gain setting for a large number of people who walked into your office with that particular hearing loss, but it should be (necessarily) understood to be the best fit for the actual individual you are fitting.

|
| FIGURE 6. The necessity to move the shadow curve into the patient’s residual auditory area. |
The correct approach is to maximize the residual hearing of the patient. We need to stop trying to “hit the target” and instead start filling the “window” (residual auditory area). To do that, we need to identify the parameters of the patient’s auditory area, including threshold and uncomfortable loudness levels at discreet frequencies. In this way, the hearing instrument becomes of most use to the patient.
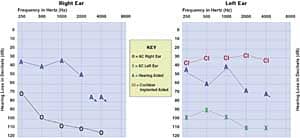
Figure 1 represents the auditory area of a normal-hearing person with shadowed area representing average conversational speech (Note: These are represented as TM dB SPL). For a normal-hearing person, the range between “just audible” and “uncomfortably loud”—what some call the auditory area or dynamic range of hearing—is quite large. Average unamplified conversational speech lies somewhere in the middle of this range. Speech is audible and comfortable across a wide frequency range for normal-hearing people. Because of this nice large range of hearing, they can experience all the dynamics (peaks/valleys, soft, average, or loud levels) of speech and music stimuli.
First-fit targets for people using hearing aids need to be modified so they can achieve complete auditory performance relative to the their dynamic range. Today’s electroacoustic technology gives dispensing professionals that ability. The hearing instrument’s electroacoustic performance should be designed to fit the psychoacoustic measures of the patient’s residual auditory capacity. This should include not only hearing threshold level (HL) data, but uncomfortable listening level (UCL) data as well. After all, the goal should ensure audibility of important sounds, especially speech, while limiting loud sounds at all frequency levels (ie, placing them below the patient’s UCL).
Figure 2 shows hearing instrument performance in this aided SPLogram. This patient’s residual auditory area is overlaid with aided speech targets in Figure 3. If you fit wide dynamic range compression (WDRC) instruments to meet gain targets, you have helped the patient hear better. Figure 4 shows correction of hearing loss based on a current gain fitting formula with a current WDRC hearing instrument. Some formulae also generate a UCL target.
To achieve the best results, we need to make new measurements that are not difficult, but are different from our standard test battery. New digital electroacoustic technology is more fully utilized, not by meeting prescriptive gain targets but by fully stimulating each patient’s residual auditory area. The major—and exciting—electroacoustic difference between analog and digital hearing instrument technology is that the hearing aid gain of digital instruments is no longer directly correlated to it’s output. Old custom electroacoustic fitting methods often compromised the required gain relative to its output, reducing it for patient “comfort”.
Remember, we should never exceed a patient’s loudness discomfort level by even 1 dB. Historically, hearing instrument returns for credit have not been due to the gain of the device, but rather because of excessive or too little output, as well as poor frequency response (sound quality).
The realization that older fitting formulae were no longer realistic targets for newer technology instruments prompted Cornelisse, Seewald, and Jamieson4 to publish an article in March 1995 that recommends using both threshold and supra-threshold hearing measurements. They suggested that the residual auditory area be fully measured and utilized for each patient. By incorporating this frequency-specific data into the custom fitting of personal amplification devices, they theorized a successful fitting.
Today’s digital technology must be custom fit to the patient’s remaining “window” of hearing ability and validated with a “family” of real-ear measurements, including RESR and REAR targets, in-situ UCL measurements, or RECD measurements. Not just a single “prescriptive” gain target will do. Taking Figure 4 as an example, the appropriate supra-threshold results should be entered into the equation not as a “formula” target but as a patient-specific UCL target.
With today’s digital hearing instrument technology, we now have a variety of adjustable response bands and compression channels, which allow our custom fitting efforts to no longer be compromised with reduced gain or excessive output as was, many times, necessary when fitting analog technology. In effect, this requires a fitting method customized for each patient’s residual auditory area or dynamic range—not his/her hearing loss. Hearing loss is just that: it’s lost and gone! A person who has lost hair cells will not get them back.
Chapter 5 of Margaret Skinner’s landmark book Hearing Aid Evaluation5 includes the basis for and description of methods for determining an individual’s auditory area. These methods utilized current testing methods and technology of that time. Today’s digital hearing instrument technology now gives us the opportunity to present precise amplification into the complete residual auditory area. Each patient’s auditory area possesses unique stimulus requirements to satisfy the patient. Therefore, each patient’s remaining auditory area should be assessed completely.
A Custom Electroacoustic Fitting
Figure 4 represents the goal of complete stimulation of a patient’s residual auditory area. The residual auditory area for each patient is defined as the difference between their air threshold scores and their uncomfortable loudness level, as measured at each octave and half-octave, beginning from 250 Hz to 6000 Hz. The test protocol for air threshold has been well defined. In Skinner’s book,5 she provides a table of estimates for MCL and UCL data as derived from threshold (HL) scores obtained from Kamm, Dirks, and Mickey.6 The measurement process should consist of an air threshold measurement using, preferably, insert earphones. Loudness growth testing should be performed at 1000 Hz, 2000 Hz, 3000 Hz, 4000 kHz, and 6000 Hz because many of today’s amplification systems possess their peak output responses at those frequencies and many hearing loss pathologies exhibit significant recruitment at those very same frequencies.
It is now possible to adjust amplification performance in 1 dB increments. Let’s fit the instrument output to within that 1 dB—not to exceed any UCL threshold by even 1 dB. We should strive to fit instruments this way—not by theory but because we can and the evidence suggests it would be greatly beneficial to the patient!
The prescriptive fitting formula shouldn’t be the critical element; the most popular ones are well tested and do an exceptional job. The critical custom-fitting component is the SPL (electroacoustical) and UCL (psychoacoustical) component of the hearing aid fitting. The patient’s residual dynamic range must be defined and fully stimulated for maximum patient satisfaction and perhaps, their auditory health (with regards to auditory deprivation). With today’s digital technology, hearing instrument gain is not necessarily compromised by its output.
Figure 6 demonstrates the necessity to move the shaded area into the patient’s residual auditory area. For a person with a moderate-to-severe hearing loss, the range between “just audible” and “uncomfortably loud” is significantly reduced. The goal in terms of fitting a hearing instrument to this individual’s ear would be to provide appropriate amplification (ie, using compression) so that speech will be audible and comfortable, and as much of the dynamics of speech will be preserved.
This fitting method addresses the gain and output parameters of instruments. However, frequency response becomes much easier to select once these two components have been defined. The frequency response slope should never exceed the slope of the patient’s real-ear unaided response.
Similarly, the frequency response slope should not (necessarily) be based on an audiogram slope. Appropriate test protocol should be followed to define the required electroacoustic response of the recommended hearing instrument. The electroacoustic response needs to be designed to fully utilize the patient’s residual auditory ability.
A threshold audiogram should continue to be defined. Frequency-specific UCL must also be determined to find the maximum output that may be introduced. This testing may be in the form of loudness growth testing through a computer, during impedance tests, noting acoustic reflexes at 500 Hz, 1 kHz, 2 kHz, 4 kHz, and 6 kHz, an audiometer at 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz using warble or narrow-band masking stimulus, or in-situ with the instrument itself. Verification and hearing-in-noise tests follow.
A computer, a tympanometer, an audiometer, and a real-ear measurement device are the primary equipment required in the custom fitting of each patient’s “auditory window.” We’ve also found it useful to observe the patient’s eyes for the ocular musculature reflex, which occurs during high intensity sound stimulus.
Today’s dispensing professional must fully define each patient’s residual auditory area and custom-fit that area completely. Current hearing instrument and diagnostic test equipment give all dispensing professionals the opportunity to truly individualize the fit for our patients—electroacoustically and psychoacoustically.
Acknowledgement
The authors thank Mary Leisses for her help with a section of this paper.
References
- Kochkin S. MarkeTrak VI: On the issue of value: Hearing aid benefit, price, satisfaction, and repurchase rates. Hearing Review. 2003; 10(2):12-26.
- MarkeTrak VII: Customer satisfaction with hearing instruments in the digital age. Hear Jour. 2005; 58(9):30-43.
- Fletcher H, Munson WA. Loudness, its definition, measurement and calculation. J Acoust Soc Amer. 1933; 5:82-108.
- Cornelisse L, Seewald R, Jamieson D. The input/output formula: A theoretical approach to the fitting of personal amplification devices. J Acoust Soc Amer. 1995; 97(3):1854-1864.
- Skinner MW. Hearing Aid Evaluation. Englewood Cliffs, NJ: Prentice-Hall; 1988.
- Kamm C, Dirks DD, Mickey MR. Effect of sensorineural hearing loss on loudness discomfort level and most comfortable level judgements. J Speech Hear Disord. 1978; 21:668-681.



.gif)
