Middle ear muscle reflexes—their generation, their measurement, and the neuroanatomy and physiology related to them—are very important in understanding the auditory system and hearing aid fittings. Once understood, they provide an excellent tool during hearing aid programming for controlling the parameters related to loudness summation.
By Jay B. McSpaden, PhD
This is the second of two articles that address the authors’ perspectives on the importance of otoimmittance measurements. The first article1 was intended as a basic introduction to the value of tympanograms relative to referring or not referring patients for medical evaluation. This article provides a similar brief glimpse at how dispensing professionals can use acoustic middle ear muscle reflex measurements to gain important insights into their hearing instrument fittings.
Middle ear muscle reflexes—their generation, their measurement, and the neuroanatomy and physiology related to them—are very important in understanding the auditory system. Once understood and combined with knowledge gained from tympanometry, these tools can serve as a general guide in hearing aid programming and for controlling the parameters related to loudness summation.

|

|
| Jay B. McSpaden, PhD, BC-HIS, is an audiologist, who retired from private practice and currently works as a hearing instrument specialist in Jefferson, Ore. Dana K. McSpaden, MSEd, is an audiologist and speech-language pathologist who, like her father, often teaches courses for dispensing professionals. | |
A recent Hearing Review dispenser survey2 showed that only half (50%) of all dispensing professionals routinely perform tympanometry and less than one-third (29%) performed acoustic reflexes. It needs to occur to us that, if we are not perfect every time and if there are useful and revealing tools/tests available in the armamentarium that we do not use, then we are guilty of a fault that borders on negligence.
Otoimmittance is of great value in higher-level problem-solving tasks relative to understanding a client’s hearing loss, as well as the signal processing needed. This article, as with the previous article on tympanometry, shows just a few reasons why it behooves hearing care professionals to utilize otoimmittance tools as part of their standard practice. Entire books have been written on this topic; although this article does not go into the finer points of sensitivity prediction by acoustic reflex (SPAR) and using acoustic reflex thresholds (ARTs) as a predictor of hearing loss, it is meant to encourage readers to investigate these topics further.
Acoustic Reflexes and Hearing Aid Fittings
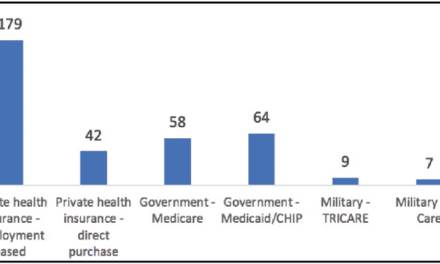
Acoustic reflexes are triggered by the summation of sufficient motor neurons—in the arc of afferent VIIIth nerve to efferent VIIth nerve along the VIIth nerve pathway—to gather and fire in response to perceived loudness (Figure 1). The reflex is caused at the point in loudness summation where the ear “goes non-linear.” Behaviorally speaking, this point is known as the uncomfortable loudness level (UCL).
In single-decibel steps, acoustic reflexes can delineate the ceiling of the individual’s dynamic range, and therefore establish the upper margin of the frequency-specific residual auditory area. It is typically measured at 250 Hz, 500 Hz, 1000 Hz, 2000 Hz, and 4000 Hz contralaterally (in dBHL), and ipsilaterally (in dBSPL) due to the calibration differences for 6 cc and 2 cc couplers. (It should be recognized that other frequencies could also be used.)
In addition, broadband noise (BBN) and/or one-half of broadband noise (BBN/2) can also be used as an acoustic middle-ear muscle reflex generator. The reflex cannot be generated at less than threshold plus 25 dB. Because the maximum output of most devices is 110 dBHL, the most severe loss possible—regardless of the “amount of recruitment”—at any given frequency would be a sensorineural (cochlear) loss of 85 dB. Mathematically, this is the maximum. Even then, it presupposes a perfectly normal “Type A” tympanogram with no history of middle ear pathology, influences of drugs, etc. (Author’s note: Years ago we performed tympanograms and acoustic middle ear muscle reflexes on drug addicted patients. If they were taking their methadone and following their doctor’s directives, they would have a “normal” or “Type A” tympanogram and reflexes. Certain drugs like heroin, however, suppress the central nervous system and the reflexes disappear. They took these tests every morning, and if the reflexes were present, they could go to work; if not, they received a lab test for drug use.)
Some of the first acoustic reflex systems were available at the VA clinic in Houston where the first author worked during the early 1970s. Early study of all aspects of otoimmittance established that any case in which the threshold of hearing approached the ART within 65 dB had to involve recruitment. Further, while a tympanogram is a measure of the physical function of the middle ear, it is not a test of hearing. Middle ear muscle reflexes are based on loudness perception and are a true test of hearing.

|
| FIGURE 1. The anatomy of the stapedial reflex arc as described by Erik Borg in 1973.3 VCN = ventral cochlear nucleus; TB = trapezoid body; MSO = medial superior olive; Nc7 = nucleus of the 7th (facial) cranial nerve. |
Acoustic middle ear muscle reflexes require hearing, but they are not a substitute for hearing testing. However, we can obtain some understanding and a “glimpse” of what the audiogram might look like through these measures. Thresholds for tones establish the floor of the residual auditory area. In contrast, reflexes for tones establish the UCLs, or the ceiling of the residual auditory area.
It is important to plot the reflex thresholds as an “R” with a circle around it at frequency, and intensity. The acoustic reflexes using speech are at MCL (either aided or unaided). Plotting these on the audiogram allows the identification of recruitment by inspection. This kind of information, when used properly, permits us to begin with a physiologic base for our work and may be the ultimate starting point for evidence-based practice.
Critical to the issue is the fact that patients do not have to be awake, alert, or even conscious for reflexes to be used. Unless there is trauma-generated or medication-induced central nervous system suppression, the reflexes will be present and measurable.
In the late 1970s, there was an effort to predict thresholds by category from the reflexes by James Jerger, PhD, and his staff. Although the effort was abandoned due to excess variability, a general prediction of the slope and configuration of the loss is possible. If you use BBN/2 for Low Pass response and subtract the reflex for BBN/2 High Pass response, the closer the difference is to zero, the “flatter” will be the mid-range of the audiogram.
Note that recorded voice speech at 1 meter played at 60 dBSPL at ear level is 40 dBHL. At that presentation, the volume of a digital instrument can be modified until an aided MCL is identified. From there, programming modifications could be done, returning to MCL in the brain. Each time, this provides a step-by-step rationale for understanding loudness and defining the dynamic range of the individual—rather than through serendipity. (The reader is also referred to the many excellent publications by James Hall III, PhD, on acoustic reflexes and predicting hearing loss from ARTs.4)
Final Notes
Our ability to function as a cartographer of the auditory system and to identify and locate the “focus” of an individual’s hearing loss transforms what we do from mere diagnostics into “physiologic geography of the auditory system.” It should be recognized that we do not tell people what the lesions are (only the pathologist can do that); however, we can tell people where the lesions are.
There are a number of causes for the absence of acoustic middle ear muscle reflexes. These include:
- Mild conductive loss <10 dB in the ear with the probe;
- Mild conductive loss <25 dB in the ear with the signal;
- Sensorineural loss in excess of 75 dB in the ear with the signal;
- Central problem with or without sensitivity shift (hearing loss);
- Any combination of the above.
Barring these conditions, any absence of reflex must have occurred for physiologic reasons. Those reasons are always related to the anatomy/physiology of the auditory system. With “Type A” tympanograms and reflexes present at normal levels, there can be no conductive component to the hearing loss. Therefore, there is no reason for bone conducted threshold measurements as they are redundant. These measures when done properly are far more accurate than any bone conducted test. Bone conduction thresholds are calibrated in 5 dB steps with 2.4 dB of freedom on either side, using an accelerometer and relying on oscillator placement on the “flat surface of the mastoid” (assuming you can find one). In light of this fact, “precise accuracy” in these measurements might be viewed as an oxymoron.
Frankly, it puzzles me why more hearing care professionals do not utilize tympanometry and acoustic reflex testing on a routine basis. Doing things right the first time should be the plan, not a surprise result!
References
- McSpaden JB. Basic tympanometry in the dispensing office. Hearing Review. 2006;13(12):16-28.
- Strom KE. The HR 2006 dispenser survey. Hearing Review. 2006;13(6):16-39.
- Borg E. On the neuronal organization of the acoustic reflex: a physiological and anatomical study. Brain Res. 1973;49:101-123.
- Hall JW III. Predicting hearing level from the acoustic reflex: a comparison of three methods. Arch Otolaryngol. 1978;104:602-605.
Correspondence can be addressed to HR at [email protected] or Jay B. McSpaden, PhD, at .