Sound stimulation delivered by open-fitting hearing instruments (OHI), combined with Tinnitus Retraining Therapy (TRT), was able to provide successful results within relatively short period of time (average: 6.9 months). OHI appears to be an effective solution for sound enrichment in TRT for mild and moderate sloping hearing losses, and could substitute artificial sound generation in many cases.
Towards the end of the 1980s, a neurophysiological model of tinnitus was proposed, which eventually led to the development of Tinnitus Retraining Therapy (TRT). TRT is based on habituation of the perception of tinnitus.1-5 This model postulates that there is an interaction between specific structures of the central nervous system, which, together with the cochlea and the auditory pathways, play a fundamental role for the appearance of tinnitus. Other systems, particularly the limbic and autonomic nervous systems, are responsible for the annoyance induced by tinnitus.2,6
TRT uses a combination of low-level broad-band noise and counseling designed to help the patient learn how to deal with their tinnitus better. Masking and TRT are similar in that both treatments introduce sounds to patients. Maskers emit sounds that either partially or completely cover the sounds of tinnitus, while TRT sound generators emit a quieter sound that allows the tinnitus to still be heard. Maskers are meant to provide immediate relief from the perception of tinnitus, while TRT and its use of sound generators are accompanied by “directive counseling.” Unlike the immediate effectiveness of masking, TRT can sometimes take as long as two years to be achieved. However, TRT can be very helpful for some patients.
Tinnitus appears when the external stimulation level is reduced, and the signals—previously processed as random spontaneous activity of the auditory pathways and filtered without reaching the level of conscious perception—start being perceived at cortical level.7
The rationale of TRT is to induce and facilitate habituation of tinnitus using an approach that relies on two fundamental aspects of brain functioning:
1) Habituation of the reaction of the limbic and sympathetic system.
2) Habituation of sound perception allowing the patient to ignore the presence of tinnitus.
To make habituation easier, retraining counseling and sound enrichment are administered. When tinnitus signals are presented to the nervous system together with a background noise signal (sound enrichment), the perception is less intense and more difficult to detect. This is the rationale for the use of sound enrichment devices in TRT.
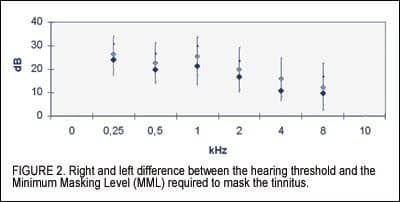
Patients with tinnitus very often have mild to moderate hearing losses8 typically at frequencies higher than 1.5 kHz-2 kHz and with limited associated hearing handicap. The pitch of the tinnitus is often found in the frequency range of 3 kHz to 8 kHz. Furthermore narrowband noise exceeding the audiometric threshold with 10-15 dB is often enough to mask the tinnitus at the pitch frequency.
Because open-fitting hearing instruments (OHIs) do not occlude the ear canal significantly, and therefore do not induce any major sound attenuation, good amplification within the 2-6 kHz band can be achieved, supported by effective anti-feedback systems.9 This is one of the main reasons why open-ear aids are regarded as acoustically “transparent” and perceived highly comfortable by patients.
Based on this, it is reasonable to assume that OHIs can provide exceptional amplification characteristics for the sound enrichment supporting TRT. The aim of this investigation was to assess the efficacy of sound enrichment with OHIs in connection with TRT.
Methods
A total of 22 subjects from our pool of tinnitus patients meeting the following requirements were randomly selected for inclusion in the study:
• Tinnitus not associated with hyperacusis.
• Falling within Jastreboff’s tinnitus category 1 and 2 and with hearing loss in the 2-6 kHz frequency range.1
• Disabling tinnitus based on the Tinnitus Handicap Inventory, with THI scores of 38 or more.10
• Willing to attend regular follow up visits.
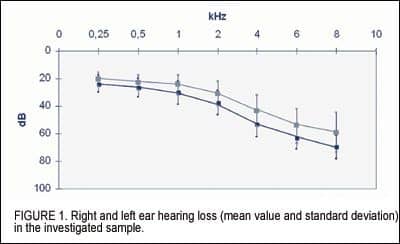
Mean hearing loss and the standard deviations for the 22 subjects are shown in Figure 1. Furthermore, the Minimum Masking Level (MML) test11 showed that, very close to the pitch frequency of the patients’ tinnitus, narrow-band noise exceeding their audiometric thresholds by approximately 15 dB was often enough to mask their tinnitus (Figure 2).
All patients followed the TRT diagnostic and rehabilitation protocol, which includes:
1) Initial examination and ENT medical evaluation.
2) Pure tone and speech audiometry, tinnitus measurement, impedance measurement, and high-definition DPOAE (10 pp/octave). If necessary, ABR, Eco-G, or MRI tests were also administered.
3) Initial administration of the structured interview5 and the THI self-administered questionnaire.10
4) Counseling and administration of a therapeutic protocol including environmental sound enrichment device for use during sleep and OHI fitting for use at least 8 hours/day.
5. Follow up visits, counseling, and check of hearing instrument fitting after 1 month and subsequently after 3 months.
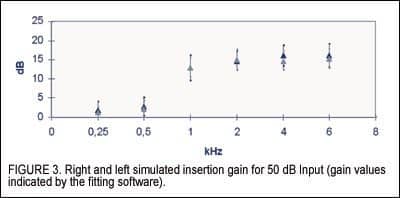
The OHIs were fitted to one ear in 14 patients and to both ears in 8 patients. In unilateral fittings, the hearing aid was applied to the side with tinnitus and hearing loss. In bilateral fittings, tinnitus was perceived centrally and there was a bilateral hearing loss. For 19 patients, ReSoundAIR and ReSoundAIR Plus were used, and for 3 patients the Widex Diva Elan was used. The applied amplification as indicated by the fitting software is shown in Figure 3.
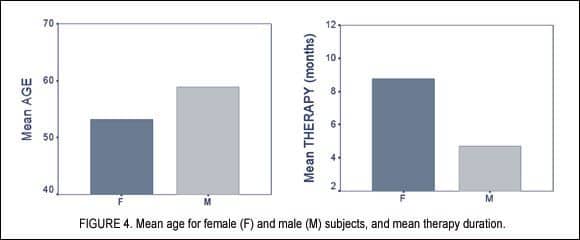
For the assessment of the efficacy of tinnitus treatment with OHIs, we have collected data through structured interviews and questionnaires (Tinnitus Retraining Therapy and Tinnitus Handicap Inventory) administered upon the first visit and at the follow-up visit after a mean number of 6.91 months (SD=3.37) (Figure 4).
Results
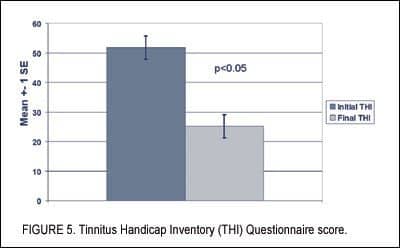
The key result was a reduction in the overall score obtained from the THI questionnaire, decreasing from 51.82 to 25.18. This reduction translates into a shift from a moderately severe to severe condition to a mild condition, according to the Tinnitus Handicap Inventory (THI) questionnaire scale (Figure 5).
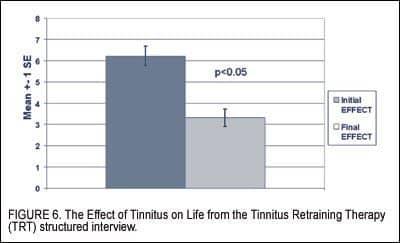
Concerning the effect of tinnitus on life—as assessed by the 0-10 scale of the TRT questionnaire—there was a change from 6.23 to 3.32—a significant reduction (Figure 6).
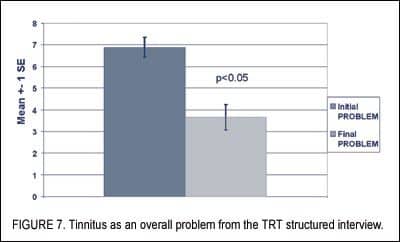
Similarly, tinnitus as an overall problem decreased significantly from 6.89 to 3.66 in the 0-10 scale of the TRT structured interview (Figure 7). Data normality was verified by the Kolmogorov-Smirnov test. The group comparison (before versus after) was statistically significant (p<0.05).
Conclusions
The aim of this study was to assess the efficacy of sound stimulation delivered by open-ear hearing instruments (OHIs) for tinnitus treatment using Tinnitus Retraining Therapy (TRT). Tinnitus patients falling within Jastreboff’s tinnitus categories 1 and 21 and with mild moderate hearing loss in the 2-6 kHz frequency range were included in the study. The results collected through the questionnaires show that the sound stimulation delivered by the OHI combined with TRT was able to provide successful results within relatively short period of time (average: 6.9 months). Therefore OHI seems to be an effective solution for sound enrichment in TRT for mild and moderate sloping hearing losses, and could substitute artificial sound generation in many cases.
The transparency of amplification and listening and wearing comfort provided by OHI allow the patient to “forget” wearing the hearing aid. Furthermore, the “invisibility” of the hearing device12 is a very important element in TRT.
The questionnaire results show the combination of sound stimulation delivered by the open hearing devices and TRT successful create results even in relatively short periods of time (eg, average of 6.9 months). Based on these data, OHIs appear be an effective tool for sound enrichment in connection with TRT for mild and moderate sloping hearing losses, and these hearing aids also seem to be able to substitute custom sound generators.
The results will soon be verified in a multi-center and multilingual study.
Acknowledgements
The results from this paper were presented at the 29th annual Mid-Winter Research Meeting of The Association for Research in Otolaryngology (ARO), February 5-9, 2006, in Baltimore. The researchers are currently preparing a follow-up multi-center study that includes universities in the United States. This research has been partially funded by the Tinnitus Research Initiative.
References
1. Henry JA, Jastreboff MM, Jastreboff PJ, Schechter MA, Fausti SA. Assessment of patients for treatment with tinnitus retraining therapy. J Am Acad Audiol. 2002;13(10):523-544.
2. Jastreboff PJ. Phantom auditory perception (tinnitus): Mechanisms of generation and perception. Neurosci Res. 1990;8:221-254.
3. Jastreboff PJ, Hazell JWP. A neurophysiological approach to tinnitus: Clinical implications. Brit J Audiol. 1993;27: 7-17.
4. Jastreboff PJ, Hazell JWP, Graham RL. Neurophysiological model of tinnitus: dependence of the minimal masking level on treatment outcome. Hear Res. 1994;80,216-232.
5. Jastreboff PJ, Hazell JWP. Tinnitus Retraining Therapy. Implementing the Neurophysiological Model. Cambridge: University Press; 2004.
6. Snow JB Jr. Tinnitus: Theory and Management. Hamilton: BC Decker Inc; 2004.
7. Jastreboff PJ. Tinnitus habituation therapy (THI) and tinnitus retraining therapy (TRT). In: Tyler RS, ed. Handbook of Tinnitus. San Diego: Singular Publishing; 2000:357-376.
8. Hiller W, Goebel G. Assessing audiological, pathophysiological, and psychological variables in chronic tinnitus: a study of reliability and search for prognostic factors. Int J Behav Med. 1999;6(4),312-330.
9. Kiessling J, Brenner B, Dyrlund O, Jespersen CT, Groth J. Occlusion Effect of Earmolds with Different Venting Systems. J Am Acad Audiol. 2005;16:237-249.
10. Newmann CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122(2),143-148.
11. Tyler RS. Tinnitus treatment. New York: Thieme Medical Publisher; 2005.
12. Johnson CE, Danhauer JL, Gavin RB, Karns SR, Reith AC, Lopez IP (2005). The “hearing aid effect” 2005: A rigorous test of the visibility of new hearing aid styles. Am J Audiol. 2005;14(2),169-175.
Correspondence can be addressed to HR or Luca Del Bo, Via Lanzone 36, 20123 Milano, Italy; tel: 02-48011361; e-mail: [email protected]; Web site: www.sordita.it.
Umberto Ambrosetti, MD, and Enrico Fagnani, MD, are researchers at the IRCCS Fond Ospedale Magg Policlinico, Audiology Department, in Milan, Italy; Matteo Bettinelli, MSc, Luca Del Bo, MSc, and Emanuela Domenichetti, MSc, are audiologists at Del Bo Tecnologia per l’Ascolto in Milan; and Alberto Scotti, MD, is a researcher at the Ospedale S. Paolo clinic in Milan.